Ayla’s VBAC Birth Story
On Thursday 12th September at around 12.30 am, at 39+4 weeks pregnant, I waddled upstairs to try to get some sleep. As I laid down, I heard a very loud pop.
That’s weird I thought.
At first, I thought something had burst in my belly, but when I went to the toilet, I experienced trickling that didn’t stop.
I went downstairs to tell my husband I thought my water just broke. Hubby, who was still absent-mindedly watching TV, had heard my self-diagnosis three times already in the pregnancy, so he double-checked I hadn’t just peed myself again. But, as soon as he finished that sentence, more liquid trickled down my leg.
Hubby gasped and agreed that my waters had broken.
It took hubby about 30 seconds to grab a towel, but by the time he had returned, I had a puddle on the floor and my knickers were soaked through. I called my parents to ask if one of them could look after our older two boys, as they were asleep and they had school the next day.
My dad came over and asked me if I was in any pain. I wasn’t but I was experiencing quite a bit of cramping, which I had put down to Braxton Hicks. We called the triage first and they confirmed that it sounded like my water broke.
“Have you got any pain?”
“No.”
“Are you experiencing contractions?”
“I don’t think so. Tightenings possibly but nothing that’s painful to write home about.”
“You better come in.”
As I was considered high-risk due to my miscarriage previously, I had to come in as soon as my water broke.
Off to the hospital
I grabbed my hospital bag and we headed to triage and the midwife asked me to keep a pad on, so she could check whether it was amniotic fluid and not just pee.
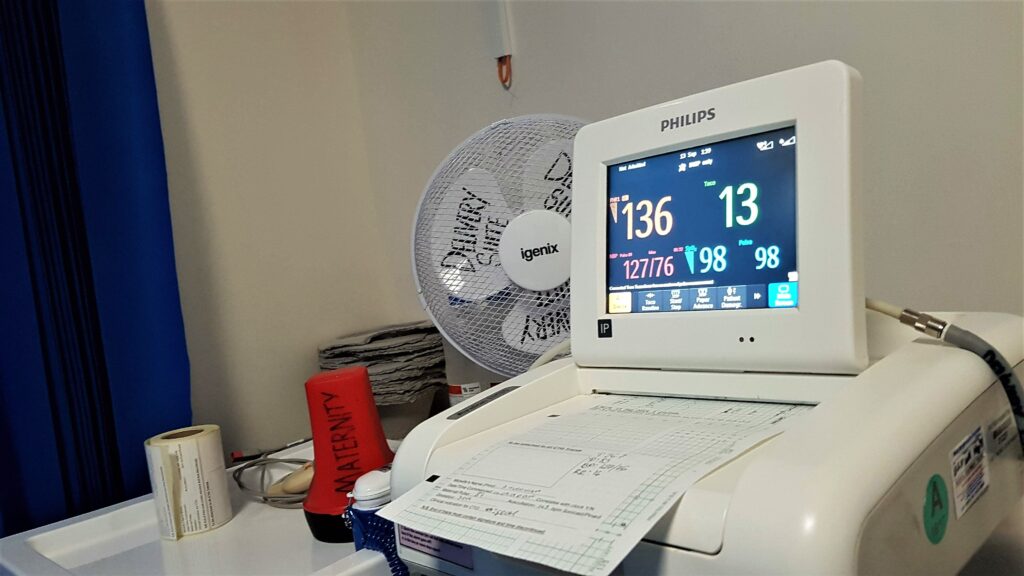
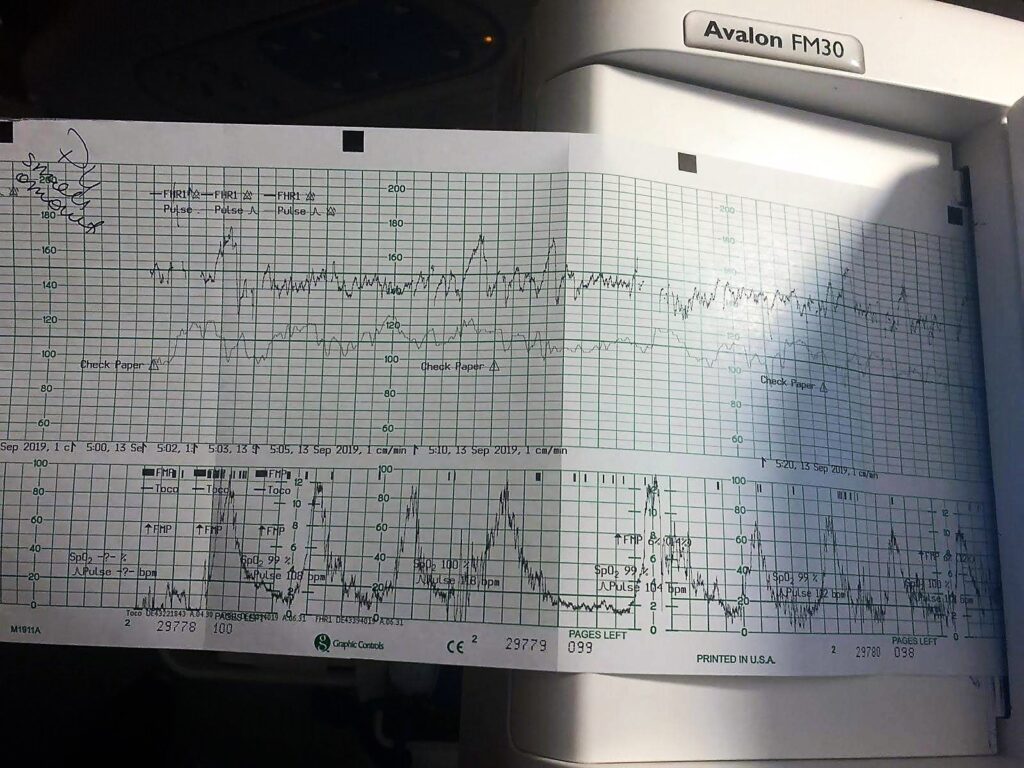
I laid on the bed as the midwives tested the liquid with a speculum, and they confirmed my waters had broken. A CTG was strapped to my belly to monitor the contractions, which I was experiencing regularly at this point. I thought this was strange because I wasn’t feeling any pain. After about half an hour to 40 minutes of checking, I was famished so I asked hubby to get me a sandwich.

I had to have an IV drip put in for Group B Strep antibiotics to be administered because I was tested positive for Group B Strep in 2017 when I had my miscarriage. The cannula put in was quite painful, apparently because my veins are really juicy and I had holes or waves in the veins. The midwife found air I think and so she had to take it out and put it on the other hand, which hurt a lot!
The two midwives in the room advised they were going to take me upstairs to the delivery suite soon. I was still fine and not experiencing that much pain until I was told to lie down. I told the midwife that I wasn’t comfortable with lying down on the bed and asked whether I could still be active. The midwife responded that when they took me to the delivery suite a bit later I would be able to move around then, but they had to continuously monitor me right now to check if the baby was ok.
It took a while for all the checks to be done and I felt so uncomfortable. The pain of some contractions was seeping in too, but I got the go-ahead to be moved to the delivery suite.
Off to the delivery suite
When I got to the delivery suite, a midwife examined me and she said I was 2 cm. The contractions were nothing to write home about; I could still talk, and I had some time in between them but they were starting to get a bit painful.
The midwives found me a birthing ball, but I still had a CTG strapped to my belly because they wanted to monitor my contractions and the baby’s heart rate, which was still high up on the 130/140 range.
We sat around and walked around a bit and I was advised not to eat in case I had to go to the theatre. I had a previous emergency c section and a planned c section, but I had made it very clear from the offset that I wanted to have a vaginal birth this time. I wanted to go as far as I could before the option of theatre had to come in. So I stuck my earphones in and listened to my hypnobirthing tracks. I kept concentrating on two chants I learned during my hypnobirthing course;
“Contractions are not that painful.”
“Your body can do this.”
I got into a rhythm of breathing in and out through the labour track while repeating the two chants in my head and I felt the process calmed me down.
Labour started and the pain increased steadily. The midwife asked me if I would consider having an epidural during this birth. I honestly didn’t know, but I said I would like the option. So the midwife brought the machine in.
The contractions were escalating now but I realised the pain was all in my back. I got really annoyed because I thought this baby was in an optimal position. I actually think she was in an optimal position until I got to the delivery suite because the contractions had changed drastically. I wasn’t feeling any contractions before 2cm. But, once I got to about 4 or 5cm, all of a sudden it felt like someone had stamped on my back and the pain was ongoing.
The midwife said she was going to try to turn the baby. So she got me to lie on the bed, which I didn’t think I could do because I was in so much pain. She assured me that lying on my side would take the tension off my back. She gave me some gas and air and told me to breathe in and out.
The midwife bent my inside leg and placed my foot on the floor and then she pushed against my back. She said we had to do this for three contractions and then we would turn to the other side.
It did feel like the pressure was off for a bit. The contractions were obviously still painful but they weren’t as painful as they were when I was walking around. When the midwife kept telling me to get on the bed, to rest a bit, I couldn’t. I couldn’t sit down, I couldn’t lie down. The only way I could lie on my side was when the midwife was pushing against my back.
We did that for three times each go, but when I had the next contraction, the pain was worse. She apologised for the manoeuvre not working. Well what can we do, I thought. It’s just the way it is. So I carried on trying to find a way to be one with the pain.
Then there was a shift change. A lovely very experienced midwife called Jo asked me whether it was ok to have a student midwife join and observe and I said yes, that’s absolutely fine – four eyes are always better than two in my opinion!
Contractions are real pain!
I was starting to struggle a lot. I thought this can’t be right, why am I not feeling anything in the front of my belly? Weren’t contractions at the front of my belly?
Jo said: “It’s because you’re having back labour. And, unfortunately, with back labour, things tend to take a bit longer.”
I thought, ok well I’m not going to let that cloud me. I had 3 days of back labour with Aron which was really intense and it ended in a crash caesarean, but Jo and Alicia were very positive that I was going to have my natural birth if I found a way to calm down.
“We’re still going to have our normal birth, don’t worry. Keep going, keep trying, keep breathing. Relax, stay positive, and breathe.”
I was examined at this point and I was 7cm. The last contraction felt like it had lasted five minutes, although it was probably only about 30 to 45 seconds. I tried to breathe through the pain and I had this system where I was shaking my hands as hard as I could to try and displace the pain. It worked until 7cm but then it stopped working.
From that point, I found it very difficult to keep the momentum of breathing through the pain and found myself holding my breath and tensing up. My husband kept reminding me about the chants, so I tried to focus back to the breathing and it worked for a couple of tries.
Epidural? Yes! A thousand times yes!
They asked me again if I wanted an epidural and I kept putting it off. I kept thinking, no I’m not going to do it. But when it got to about 7cm or 8cm, the pain had doubled, and they were getting stronger and longer. I found it too difficult to listen to the track, and couldn’t breathe through the pain anymore. It was getting to about 10.30 am at this point and hubby helped me by pushing and pressing on my back, as well as squeezing on my hips, which is what the midwife showed him to do. When the midwife asked again, “Do you want to try the epidural?” I said:
“Yes, 100% yes, I want to have the epidural NOW!”
The anaesthetist was running late; he had been called to theatre due to an emergency c section. The midwife apologised and I said no, no this is a blessing in disguise in some way. I had to deal with this on my own and I needed to find my way. So in a way, I was kind of glad it wasn’t there. But, at the same time, I was also thinking my gosh this is real pain.
So I must have got to about 8 cm, I wasn’t checked, but the contractions were coming hard and fast now and they were so painful. Then all of a sudden the anaesthetist turned up. The two midwives kept telling me:
“Come on, you can do it. Breathe! Breathe!”
They were really positive; they were breathing with me and rubbing my back. They were doing everything they could to try to get me to relax. And it worked for a while; I got into the zone a little bit. The anaesthetist again asked if I wanted the epidural and I didn’t hesitate. I screamed:
“Yes, I want the epidural! I can’t take this, it’s too much pain!”
I was given a button and advised that the epidural would need to be topped up every 25 minutes, although the pain wouldn’t necessarily come back in 25 minutes. So I was told to only press the button if I was in pain. So, from that point, I tried to challenge myself to not press the button as long as I could.
And sometimes I could feel the edge of the contractions coming back and then I’d wait for the next contraction before I pressed the button, or I’d wait until two contractions before I pressed. It was like my own private challenge to help me get through it. Plus, it was taking my mind away from how long everything was taking.
Every contraction gets you one step closer to your baby
I remember in the hypnobirthing course, Dani Diosi the course creator, said every contraction is getting you one step closer to your baby. So all you’ve got to think about is that you’ve done one, you’ll do another one and it’ll be one less than you’ll need to do. So I kept trying to think that way.
Every time the button came on I tried not to look at the green light. Jo advised me to be careful when I got to the pushing stage because I’d needed to stop topping up so I could feel the pressure to push.
I thought because I was still feeling the pressure of the contractions, I didn’t think it would make any difference.
Jo examined me and said I was at 9cm now.
Wow, that’s brilliant! I’d never got to 9cm before! I only got to 6cm with my first and my second was a planned c section, so I was in unchartered waters now.
I was so happy. I managed to get a little nap in as well and the midwives kept my mood up by joking around. At one point my husband said he was getting cramp from waving the fan to cool me down and Jo asked if it was ok to evict him from the birthing room or throw him out of the window.
I laughed and said:
“No he can keep fanning me, cramp and all!”
We joked briefly about how men think labour pain is like a toothache or adult colic and it relaxed me a lot.
We’re ready to push!
Jo reckoned in an hour’s time I would be at full dilation and once I got to 10cm, I was asked to rest a bit. When I got my contraction, Jo would ask me to push when I felt the pressure. Ok, I thought, sounds straightforward enough! So I topped up one last time, and we waited for about an hour. Jo checked me and said:
“Right, you’re ready to push. Let’s go! Wait for a contraction and then push down on your bottom.”
It was then I realised oh my gosh, it is really difficult to push without the pain or pressure because there wasn’t as much pressure as I thought there would be. I didn’t realise what Jo meant when she said it would be harder with the epidural.
Jo said, “Well 50% of women who have the epidural can’t push and 50% of women who can push end up with having an instrumental delivery because they can’t feel it.”
And I thought that was a silly mistake to accept the epidural in hindsight. If I had thought about what she had said and how difficult it was to push because of how desperately I wanted to have my baby naturally, I would have refused the epidural.
That was the first time I had kicked myself because I found pushing really difficult. I kept looking at the machine to check when I was having a contraction just in case because Jo said there was no point in pushing without a contraction because the baby wouldn’t come through.
So I pushed for about an hour. I didn’t know if I was making any progress, and I’m pretty sure I pooed at that point, but they didn’t tell me.
“Don’t worry, doesn’t matter, not thinking about it,” they said.
But I’m pretty sure I did.
Jo said, “Well baby is coming slowly but she’s coming.”
It got to just about before the hour, around 40 – 45 minutes when the doctor came in and said:
“Listen, at this point baby is doing absolutely fine, there is no distress on the heartbeat, contractions seem regular, and there doesn’t seem to be a problem.”
There was an issue at one point during the pushing stage when the contractions had faded a little bit and so Alicia brought a gauze with clary sage to trigger the contractions. I couldn’t have syntocin (to be induced) because of the previous births and risk of uterine rupture. So instead of syntocin, we went for something natural. The clary sage was so strong, but the smell was lovely. And it worked! The contractions came back really hard and fast, so I kept using the contractions to push as hard as I could and Jo kept saying, that baby’s making progress – just slowly.
The doctor continued, “We have to limit your pushing to an hour before we have to prep you for theatre in case the pushing doesn’t work.”
So the next part of the pushing had to happen in theatre and not in the delivery suite because the doctors had to make sure that if anything happened they could perform the c-section as soon as possible. The doctor examined the baby and he said that baby seemed fine. So they said to keep going with the pushing, but in about five minutes they were going to take me up to the theatre.
Off to the theatre
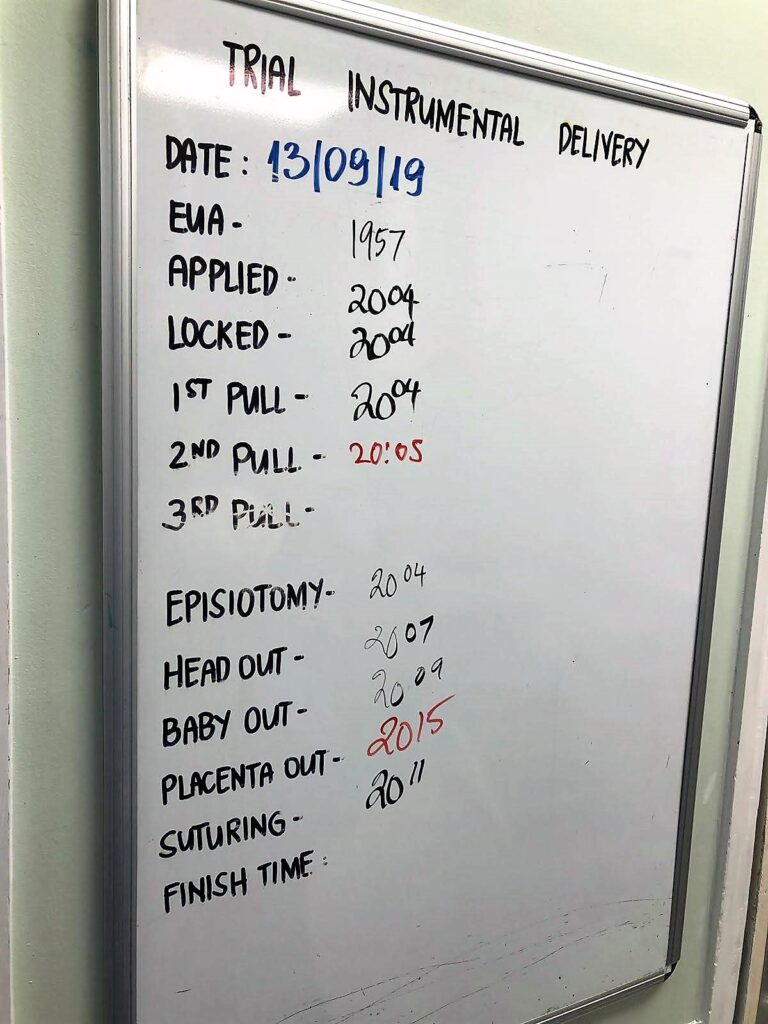
We got to the theatre and there were so many people there – so many staff and I didn’t know who they were. People kept coming and talking to me and they explained they were going to administer an epidural with a local anaesthetic so I couldn’t feel anything.
I had the checks done to see if the epidural was working and it hadn’t gone up to the chest – it’s a freezing cold test where they sprayed freezing cold water on my legs. The water felt warm until they sprayed on my chest which felt freezing cold. That meant the epidural was working fine. There was a situation earlier where on one part of my body, I could still feel the pain of the contractions so I was still taking in gas and air even though the epidural had kicked in. So Jo advised that the next time I topped up, I moved to the right-hand side of my hip so that the epidural drug filtered through.
In theatre, I was administered a local anaesthetic. The doctor advised that we were going to try pushing for a while, even though it wasn’t looking likely and we may end up with a c-section.
It was at that point I lost it. I just, I couldn’t hold back the tears. I was so upset that people kept asking me if I was ok. I said I really wanted to have a normal birth and at this point, this is where the two midwives really shone.
They really championed for me. I didn’t know about this but after the birth, my husband told me that the surgeon had been tugging with forceps to get the baby out. I tell you, it was even worse trying to push under a local anaesthetic. You have to try to remember the feeling of what it’s like to push, but you can’t push. I mean you cannot push!
But, apparently, it was working. Coupled with the local anaesthetic which made me shiver and feel weak, (I felt sick every time I pushed), I did everything I could to push my baby out. I had to push past the feeling of being sick, the feeling of shivering and the cold, which I later realised was down to low blood pressure.
She’s out! My baby is out!
So I thought I’m going to have to get through it, I have to push. So I did everything I could to push and finally, she was out. The relief I felt when they told me that she was out was just – it was euphoric. It’s something that I can’t explain:
“Wow, I did it! I pushed my baby out after two c sections!”
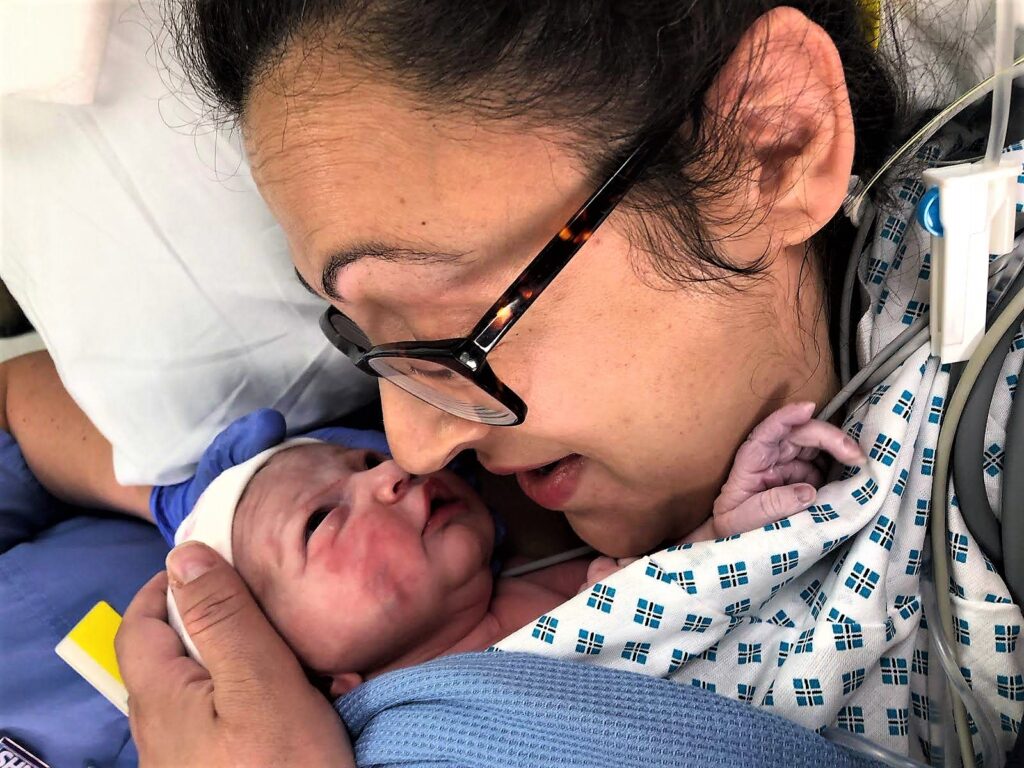
The baby wasn’t crying and she looked a little bit blue. The doctors took baby over to the examining table, straight away, and I could see they were moving her around. A few minutes later she started crying and my husband and I sobbed with relief that she’d made it. She made it through all the tugging and all this time she’d had a consistent heartbeat.
I had never felt so happy. The thought of managing a vaginal birth after two c sections was insurmountable, but I did it. I know loads of women have VBACS every day but I don’t care. For me, it was just the most immense feeling in the world.
I cried my eyes out thanking everyone in the theatre, especially the midwives.
“Thank you so much; you did it, you did it! Thank you, thank you!”
The surgeon congratulated me but mentioned it had been really tough. They had to do a forceps delivery, and I ended up with a second-degree tear and an episiotomy on each side. The midwife championed for skin on skin straight away, so while he was stitching me up I got to enjoy some really beautiful cuddles with my baby. I was so happy.

I noticed the bruises on her face from the forceps, but the doctor said not to worry as they will fade eventually. I was exhausted but I was immensely proud of myself, my body, my baby and the staff. Hubby was amazing at keeping me calm and focused too because there was one point where I thought I was going to lose it. But hubby stayed calm for me and talked me through everything. He was my absolute rock.
When they stitched me up, I got to enjoy skin on skin with my princess and they waited until the cord had stopped pulsing before they clamped and cut the cord.
They didn’t do any of the checks or weigh-ins until I had spent precious time with my baby and I thought that was amazing. It was in my birth plan, but I didn’t have to tell them that’s what I wanted.
“We don’t need to do the weigh-in checks, we don’t need to clean her now. Just put her on your skin and enjoy her.”
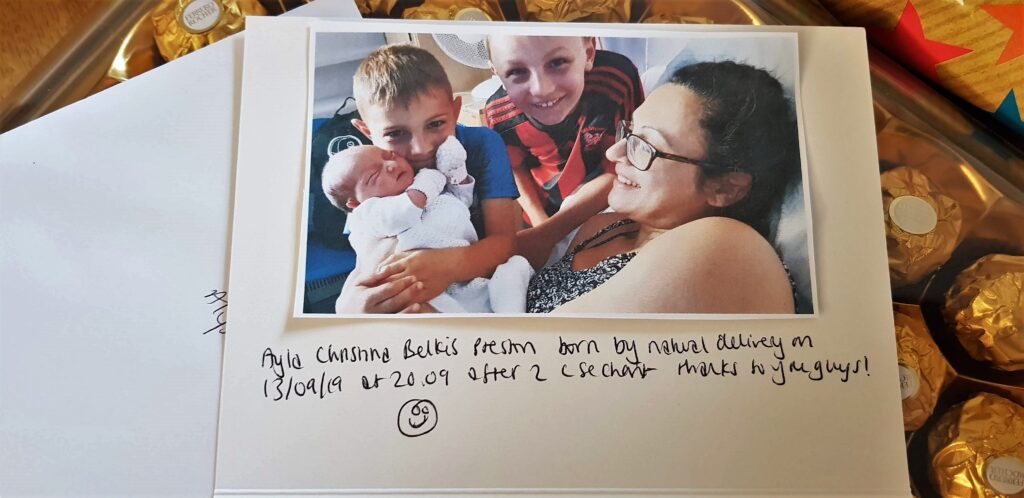
Baby was weighed at 7lbs, 7 ounces / 3.487 kg and born 39+5 weeks on Friday 13th September at 20.09. And, it was a fantastic experience!


I was wheeled into the labour ward as I was still under local anaesthetic, so I couldn’t feel anything in my legs. They put a catheter in me and I just relaxed with my baby. I was so happy she was there.

When the local anaesthetic wore off, however, oh my goodness! I was not aware of how painful birth really was! There was a swelling in my back passage, which the surgeon said I should take a look at because it could have been a prolapse. And, the afterpains, the pressure and the swelling was agonising. I couldn’t sit on my bum, I couldn’t do anything. They told me they had been giving me oramorph which was liquid morphine, but it wasn’t cutting the pain. It was getting rid of the vaginal pain but the back passage was just intense.
So, after many, many talks, the doctor decided to up the dosage. They gave me one small dose of epidural, which they tied to my back, and I scratched my back half to death because the epidural has a side effect, which is very itchy skin. I itched everywhere. It was so hot in the theatre as well, so I was sweating and so, so uncomfortable. I had also forgotten all about the bleeding aftermath.
I ate loads of food constantly. I didn’t know whether it was because of the drugs or breastfeeding, but I couldn’t stop eating. One of the midwives said I needed to let her know when I did my first poo. And I was like how the hell am I going to do my first poo, I can’t even feel that area!? She mentioned it was going to be tough because I’d had a bit of trauma down there.
I was convinced that I had over pushed and certain things had come out from the inside to the outside because of how swollen my back passage was. But apparently, you can’t overpush. The midwife assured me that the bottom will eventually heal. I asked her how long she thought it would take and she said maybe about 3 weeks; up to 3 weeks, depending on how quickly I healed. 3 weeks!? C section is 6 weeks!
She praised me again:
“Honestly, what you did was amazing, You would have not experienced the same if you had a c-section.”
She was right. It was all worth it. I had a beautiful baby out of it. So I told myself to take the pain. I’ll deal with it, just keep topping me up with painkillers!
The midwives kept asking about when I was ready to go to the toilet and and hubby desperately wanted to go home because the ward was so loud. I told him I didn’t want to go home until I hit the poo milestone, just in case I broke something else down there.
So I drank loads and loads of water, and thought about how I was going to pass this milestone with minimal disruption. The midwives advised just trying to pee first and then I thought, OMG how am I even going to pee!? The midwives took the catheter out and I thought just break the bullet; they won’t take the cannula out unless I pee.
It really wasn’t as bad as I thought it would be in terms of stinging but I was shocked at the lack of bladder control I had. As soon as I pulled my pants down it was free-flowing. I now needed to have a shower. But I thought, how am I going to have a shower!? I’ve got loads of stitches down there. The midwife told me not to use any shampoo or conditioner, I didn’t need it. I just needed to rinse off because I had been sweating buckets.
The epidural was taken off my back and it was such a relief to get all that tape off because it was so itchy. I was so sweaty, I’d actually scratched my back half to death! I had a really cold shower, which felt amazing. I felt so much better, apart from the pain downstairs.
As a result, I found it very difficult to sleep. But, the baby was amazing and she was so relaxed. We had a few problems with her latching on to the breast. She was a bit diva-like and couldn’t wait for me to show her where the nipple was – she had to have it now!
But while she was on she fed for ages and in her first night, she slept for six hours! The midwife asked me if I wanted to wake her up and I was like, do you know what? No. I think I’m just going to let her sleep, she seems fine. When she woke up, she was obviously very hungry, so I fed her again and she fell back to sleep. The poos took a while to come in but once they did she was pooing like a champion as well.
Off to the postnatal ward
The next day, I was wheeled into the postnatal ward. During the birth, I had lost 1.7 litres of blood, which is a ridiculous amount of blood to lose. I lost 900ml with my first, and 700ml with my second. I felt quite weak and lethargic – I really wasn’t feeling all too strong.
When I moved to the postnatal ward, I was prescribed iron tablets, lactulose so I could go to the toilet, co dydramol, and ibuprofen.
The consultants were worried that the oramorph was only working in the vaginal area and not in the back passage. How can liquid morphine not hit the pain in the back passage?
A consultant examined me to test whether something had happened with the epidural. They later deduced that the legs being on the stirrups may have caused some muscle tension or breakage near the hips, around the back passage and that could have been what was causing the pain. But whatever the reason was, it did not allow me to sit on my bum or lie on it.
So, I just had to lie on my the left side and very rarely on the right-hand side – it was so difficult. I couldn’t do anything. I couldn’t wait to get the next dose because the pain kept coming back.
That night my husband wasn’t around either, so I found that night really difficult. I was in a ward with two other hungry crying babies and I had to figure out how to get up off the bed, feed the baby, put her back in the cot, and then get back on the bed. So I was doing loads of ninja moves, by using my feet to control the height of the bed, the pillow area, the head area, and the headrest, and by pulling the headrest up to 90 degrees, to 45 degrees, or lying it down flat. But nothing worked. I was in constant pain.
The aftercare was amazing, though. The midwives regularly checked my obs. They also kept telling me my bloods were very low, so they might need to offer a blood transfusion. However, I said I preferred iron tablets instead, which was what I had been taking anyway.
The second night I told the midwives that my baby wanted to feed constantly and she struggled to sleep because of the other babies crying. I also found it quite hard because I couldn’t lie down with her, and I couldn’t sit up to breastfeed her. I had to do the advanced, lying-down-on-the-side breastfeeding move because I didn’t really have much of a choice.
I also found out that I couldn’t have any painkillers at night so I had to handle the pain until the ibuprofen came at 6am – I couldn’t have eaten it fast enough! Ibuprofen was the only thing that worked because it was anti inflammatory. So when I had ibuprofen, I felt relief. Actual relief.
I ate lots of food but I couldn’t go. I thought ok it’s not working so I am just going to just leave it and this really lovely midwife said to me that she’d experienced the same thing.
“Don’t push it; have Weetabix, prunes, and milk the next day and you’ll go.”
I ended up going the next day – and it didn’t hurt at all. We had lots of obs, and so did Ayla, which she passed with flying colours!
Our next-door neighbour’s husband constantly chatted on the phone in the middle of the night to his mum or family member and his baby was crying constantly. Then, when the husband went to sleep, he snored so loudly. I thought it was so selfish of him. We’ve got babies trying to sleep here and he’s chatting away throughout the night! Luckily Ayla like a champion slept really well.

I still found it difficult to sit down on my bottom, so I slept much less. The boys came to visit me in hospital and we got a lovely photo in together. They also ate all my hospital food!

Off home – with a new addition!
We took a long time to be discharged and hubby was getting restless. But, the meds had to be signed off before we were finally able to leave for home. I looked like a state when I got into the car, wearing my husband’s clothes, no makeup, and hair scrunched up on my head. I also didn’t realise that I couldn’t sit on the seat, so I had to crouch. I asked hubby to get a towel from the back, which I turned into a ring cushion and that made it much better to sit down, although the pressure was still horrible.
The first three weeks were tough but I lived on the couch with my laptop. Hubby took time off from work and he and my parents did the school run for me. It was amazing to just sit and be with my baby and I have my support network to thank for that!
I realised how important it is to have a support network around you because it can turn an otherwise positive experience into a very negative one. Hubby had to inject me for 10 days with Enoxaparin to prevent any blood clots after birth and I had to continue my meds – there were so many I had to keep to a rigorous plan, so I wouldn’t forget. I used a cooling gel for downstairs which I placed on top of my really protective pads and that really helped with the soothing and healing.
And slowly but surely, I started to heal. I was told that you will know when you’re on the road to recovery when your stitches feel really tight. I felt that around 3/4 weeks. I hadn’t used any shampoo or conditioner until that point and it felt really good to use a mild detergent like Sanex to have a proper wash. I didn’t have a bath, though, just a standing shower to ensure downstairs was free from any chemicals. I was actually very strict with my aftercare and I think that helped.
The health visitor came to check me over and asked how my mental health was. I said that I was on top of the moon! I had a really positive birth and that was a lot down to the hospital being so positive too.

I since learned that the pain of vaginal birth was probably worse than the c-section and that it didn’t matter whether you had a vaginal or a c section delivery as long as it was made to be as positive as possible. Having had both now, it didn’t matter how our babies are born. What matters are that they’re happy and healthy!
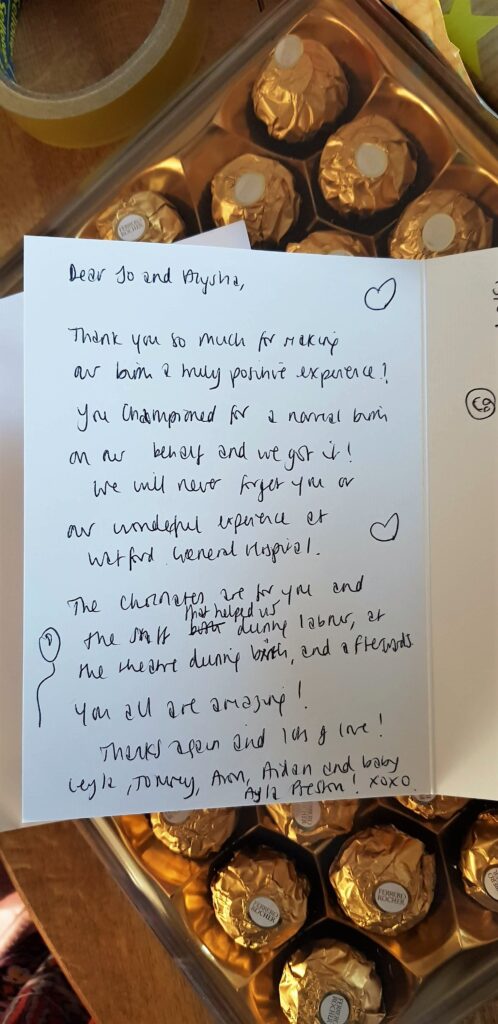
Thank you to Watford General Hospital for helping us achieve a really positive birth. We brought in some chocolates and a card to Jo and Alicia for being such amazing midwives throughout labour and birth.
A big thank you to Dani Diosi for the wonderful and very informative hypnobirthing course which helped me to think positive throughout my birth delivery and get me the positive birth I wanted and to Dr Verma for giving me hope in getting my girl. We did abandon the conception plan towards the end so it’s hard to know whether it was luck or whether Urobiologics helped me get my girl. Again looking back, it doesn’t matter to me anymore whether it’s a boy or or a girl. Being happy and healthy trumps all of it.
If you want more information on Dani Diosi’s hypnobirthing course, head here: mamaserene.co.uk
Don’t forget to read Part 1 and Part 2 of my Hypnobirthing series on how hypnobirthing works to achieve a positive birth.
If you want to learn more about how you can get the baby of your desired gender through non-invasive methods, head here: urobiologics.com
Don’t forget read the rest of my ‘Journey to getting my girl’ series here: Journey to getting my girl
Click here for more birth stories (including VBAC stories)
After a very successful VBAC birth story, I welcome Ayla Christina Preston who was born on 13 September 2019 at 20.09, two days before my due date! Ayla is now 16 months old and a very active baby!

*Some links contain affiliate links where I may earn a small commission at no extra cost to you. As an Amazon Associate, I earn from qualifying purchases.*









2 Comments