My PPROM – Second Trimester Miscarriage – Journey to getting my girl – Part 3
It has been over three years since I wrote Part 2 of Journey to getting my girl, and there is a reason for this delay.
I will get onto the reason in a moment. But, you can probably guess what it is.
So, I’m going to issue a trigger warning now:
TRIGGER WARNING! THIS POST CONTAINS PERSONAL DETAILS ABOUT MY SECOND TRIMESTER MISCARRIAGE TREATMENT WHICH MAY UPSET READERS. PLEASE DO NOT READ IF YOU ARE SENSITIVE TO THIS TOPIC IN ANY WAY.
Get an insight into your fertility with an accurate at-home test and check your female hormone levels from the privacy of your own home. Code below!
Get 25% off your LetsGetChecked Female Hormone Test with your exclusive discount code MHD25*
So, to continue with the series, we’ll start from where we left off in Part 2. If you haven’t read any of the ‘Journey to getting my girl’ series, then may I suggest you start with Part 1 here, so you understand the backstory.
To summarise, the series talks about my husband and I following a non-invasive conception plan to get our girl, using Dr Verma from Urobiologics’ two tests, the PreGender Test which determines whether the female’s menstrual cycle favours a boy or a girl via non-invasive urine sampling and the FirstGender Test which determines the gender of the baby from conception, again, via a urine sample, which claims to be 95% accurate. Urobiologics discovered that just like there are two kinds of sperm, which determine the gender of the baby, women have alternating boy-girl specific menstrual cycles, which select the gender.
We had already sent our samples in and Dr Verma emailed us our conception plan to try for a girl soon after.
The conception plan was a long, hard slog. Hubby caught a nasty flu and was out for a week, which meant we missed one month. And there was a time when we thought we may have been pregnant, but I experienced a chemical pregnancy back in May 2017, which was very disheartening, so we didn’t try the subsequent month.
But we finally got pregnant in August 2017 and Dr Verma had been so responsive during those 13 months that it felt like we had a private doctor urging us on, providing tips and tricks to maximise pregnancy.
Positive pregnancy test!
When I sent Dr Verma a picture of our a positive pregnancy test, he was thrilled for us and urged us to collect samples for three nights and ship right away so we could start the next process which was the FirstGender Test.

What is the FirstGender Test?
As soon as you get your positive pregnancy test, you ship urine samples to Urobiologics who then test to find out the gender of the baby from day 1 of conception, with around 95.5% accuracy. And they email you the results within 48 hours of receipt of the samples. You can find more information about how to book the FirstGender Test here.
Dr Verma’s emails were very detailed, informing us exactly what we should do with our samples.
“Suppose you go to bed at 10pm. Do not collect that because it is diluted. Thereafter, anytime you go to the bathroom, let it go for 2 – 3 seconds, collect in a large vessel and pick up one spoonful and add to the bottle. Discard the rest. Repeat this the whole night until morning, included. Do not collect during the day. Repeat for two more nights and then ship the bottle.”
Dr. Verma, Urobiologics
Get a comprehensive picture of your hormonal health without the need for clinics or appointments. Easy testing, free shipping, and fast results.
Order now for 25% using the discount code MHD25*
I told Dr. Verma that I wanted to keep the entire process quiet until I passed 12-weeks gestation, which he agreed and understood.
I sent the sample off within days of the positive pregnancy test and despite a slight delay thanks to UPS, Urobiologics received the sample and got to work.
My best friend was so happy for me too, bless!
Good news!
Within a couple of days, we received the email from Dr. Verma:
Ms. Preston, We are proud to be the first one to say hello to Poppy. Welcome Poppy to your home. We have completed testing of the urine sample submitted by you. The baby’s gender, as evaluated from the urine sample believed to be from you appears to be FEMALE (GIRL) with around 95% confidence, without expressing or implying any warranty. This report should be read along with the disclaimers and terms & conditions displayed on our website.
Dr. Verma, Urobiologics
We were elated. We got our girl! But we kept it quiet until the 20-week scan, just in case there were any misreadings. We were quietly confident, however, that we had our girl and we couldn’t wait to tell our family and friends at 20 weeks.
The first trimester
However, from the moment I got pregnant, I felt like something was off.
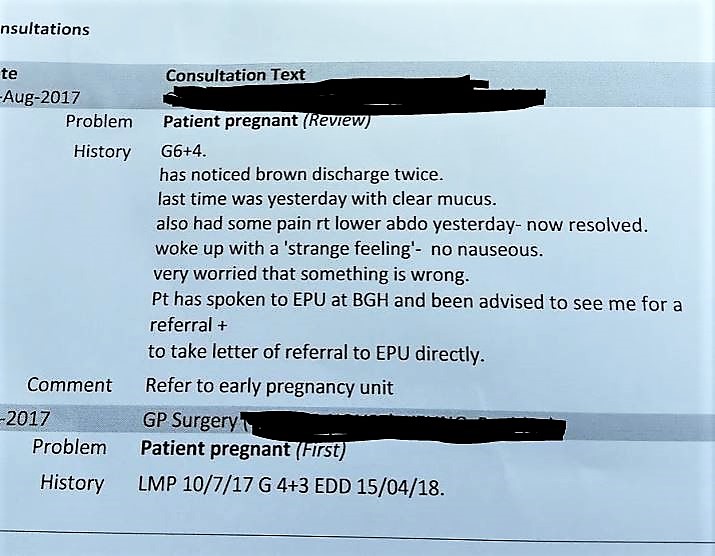
The first trimester was extremely difficult. I couldn’t eat or drink anything. I looked grey. I slept for 20 hours a day and I just felt poisoned. I struggled so much that my parents and hubby had to pick the boys up from school because I didn’t have the energy to get up. And I also had been spotting dark brown blood from week 7 to week 12 of the pregnancy.
I had a transvaginal scan at week 6 to find out if everything was ok and I saw my little dot with her beautiful little heart beating (a vision of which years later, I still see in my mind)

I was really excited to see my teeny baby beating away and sent the scan picture to Dr Verma, who said you can tell the gender of the baby by its head size, bent body (girls have a curvier backbone than boys) and the angle of the nub. He said that all three parameters pointed to a girl.
Again, we were very happy to read Dr Verma’s conditional diagnosis of the scan confirming it was a girl, but, upon reading the scan notes, again I felt like something was off.
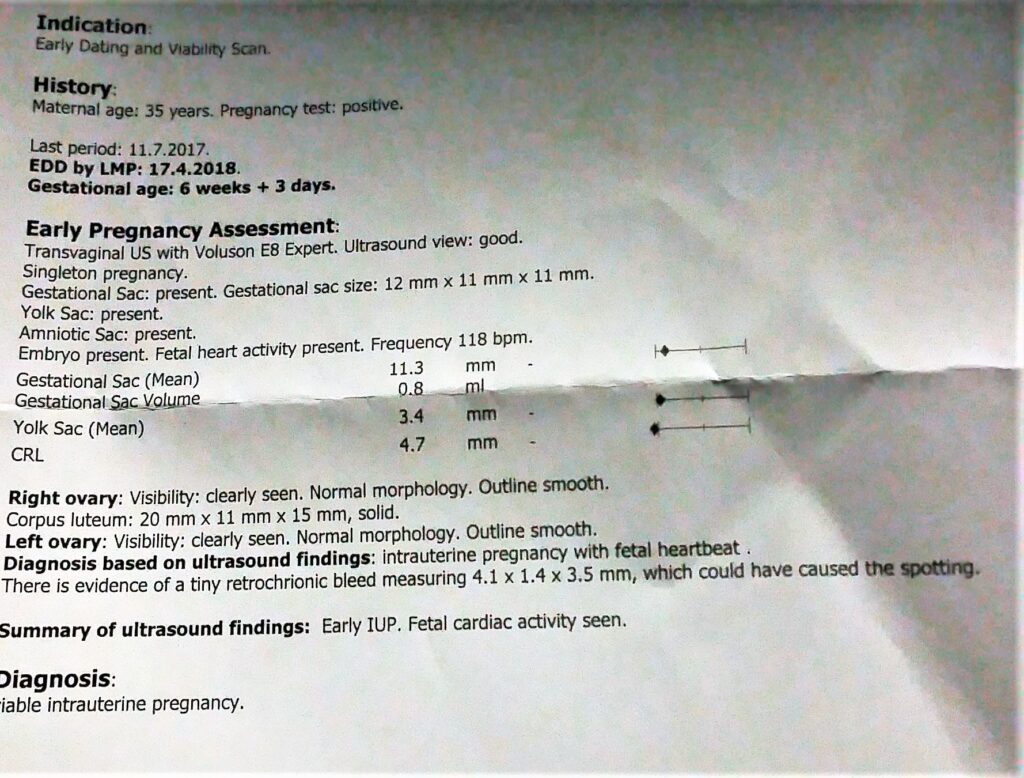
I kept thinking about whether the foetal heartbeat was a bit slow or that the size of the sac was on the small side. I thought about what that tiny retrochorionic bleed meant and why I hadn’t encountered anything like this with the boys. But the sonographer assured me it was probably down to the implantation and it would resolve itself in the second trimester. I was, however, to abstain from any form of exercise or sex and try to rest up as much as possible, which was all I could do anyway.

The second trimester
By week 13, I felt like a dark wave had lifted. The constant nausea had subsided, the spotting had stopped, and I felt more like myself again. I ventured out to Baby Shows, trips with the family and I even hosted my best friend’s baby shower – I even made a cake!



Again, I just felt off.
I was having dreams of my baby being stillborn, and friends around me were having miscarriages. I hadn’t even thought of miscarriage once with my two boys, so why was I thinking about it all the time? And, no matter how much my friends, family and doctors/midwives assured me that everything was ok, I kept thinking something was not ok.
Get an insight into your egg reserve with LetsGetChecked's Ovarian Reserve test.
Order now for 25% using the discount code MHD25*
Then the problems started
At my 12 week scan, which happened late into my 13th week, the sonographer scanned me for around five minutes, refused to answer any of my questions and treated me as if I wasn’t in the room, despite me continuously asking whether my baby was ok and expressing my concerns about this feeling I had.
She said the baby was fine and so was the heartbeat and that was that.
I called Barnet Hospital after the scan to request another, but they told me they were fully booked and that I would have had to wait until my 20-week scan to check the baby.
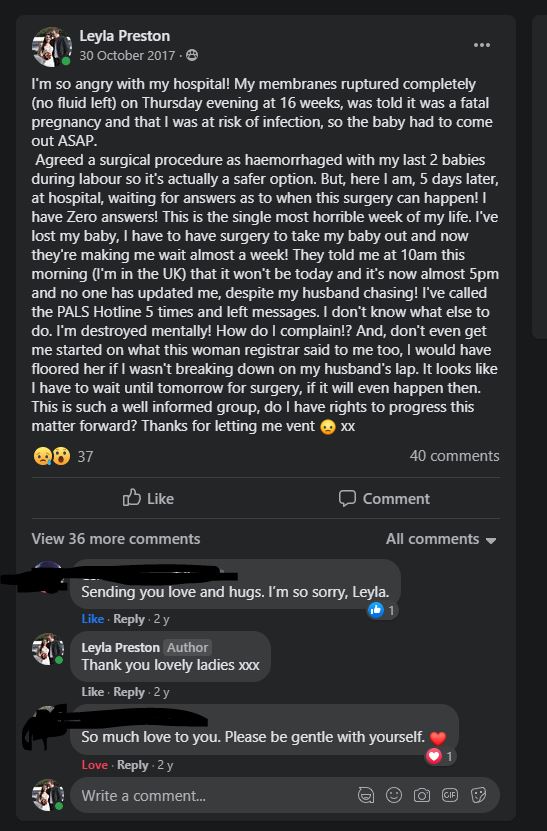
22:00 – Thursday 26th October 2017
One night, I went to the toilet and a sudden gush of liquid poured out. I first thought maybe I had peed a lot, but as I carried on with my chores, I felt trickles come down my legs. I told hubby who advised me to stop worrying, and that we’d deal with it the next day when the kids were at school. But there was no way I could go to bed. We called my dad to pop over to stay with the boys, so hubby and I could head to Barnet Hospital’s triage unit.
Off to the triage at night
The triage’s tiny waiting area was packed to the brim with pregnant couples. Some heavily pregnant women had to stand up because there was nowhere else left to sit.
I busied myself on my phone, updating my best friend on our current situation, which was nothing because nothing was happening.
23:00 – Thursday 26th October 2017
No one saw us until about an hour later when a member of staff came over and shouted:
“So, who is the 15-weeker who lost their waters?”
Both hubby and I were shocked that she had blurted our situation out in front of everyone and hubby chastised her for being so insensitive to which she apologised, but did not seem to cast another thought about it. She walked us to a large vacant room where we were told to wait until a doctor tested my waters to find out whether I had indeed passed amniotic fluid or urine.
A doctor visited briefly to ask me some questions about my past births and current pregnancy and I was advised that I would likely stay the night and await a scan in the morning to find out exactly how much, if any, amniotic fluid had been lost.
I joined tons of Facebook groups related to this Preterm Premature Rupture of Membranes (PPROM) that I had Googled, but had never heard about in my life, and there were a lot of positive outcomes of babies being born with slight complications but could still thrive despite the mum losing her waters during pregnancy.
I learned about things like bacterial vaginosis, cervical insufficiency, polycystic ovary syndrome and vaginal bleeding being causes of miscarriage, but if I had only lost a little water, I might save my pregnancy.
I had renewed hope that maybe this pregnancy was salvageable and made a silent promise to my baby that I’d do anything to save her, despite the conflicting stories on Facebook. I only hoped that I had either only lost urine, or very little of my amniotic fluid, of which I read you could replenish if you drink lots of water.
So I drank. A LOT.

00:30 – Friday 27th October 2017
A doctor arrived with an assistant to test the liquid I lost and confirmed that I had passed amniotic fluid.
Ok. Not good news, but I told myself to stay positive. Now the hope was that I didn’t lose a lot.
We were told we would have to wait to be seen by a consultant obstetrician to find out what our options were and how much had been lost.
02:00 – Friday 27th October 2017
A Mister Consultant Obstetrician came to examine me further and provide antibiotics, which he advised was to prevent infection to me and the baby. Again I was told I would have to stay the night (at 2 am I bloody hoped so!) and that they would take me for a scan at 9 am the next morning to check how much waters had gone.
If there was only a little water lost, there may be a chance to save the pregnancy and stay on bed rest to protect the baby. But if all waters had gone, then it would become a fatal pregnancy and my only options as advised was a natural miscarriage, where I would have to wait for nature to take its course and I lose the baby, or a D&E which is a Dilation and Evacuation and I would lose the baby.
I later found out that very few doctors perform this surgery because of the size of the baby and that their bones would need to be broken for the evacuation to take place. This was explained to me by a doctor during my week in hospital by the way, which is so traumatising to hear! A D&C or Dilation and Curettage is not possible on babies over 12 weeks.
The thought of my baby being broken finished me and I spent the rest of the night crying into hubby’s arms. Either way, the outlook was bleak and so I hoped that my only chance was that not all waters had gone and that there was a way to save my baby whom I could feel move but the movements were getting slower and fewer and far between.
09:30 – Friday 27th October 2017
I was transferred to the Victoria Ward, which was the delivery suite where mothers were giving birth to newborn babies throughout the day and night. The sound of new babies being born was soul-destroying because I knew there was a good chance I wouldn’t get to see mine.
So, why were they keeping me in the delivery suite!?
11:15 – Friday 27th October 2017
Two doctors came to discuss my options again and urged me it’s safer to go into natural labour. After speaking with my best friend at length, who had a D&C after a missed miscarriage at 12 weeks, I decided I was going to take the D&E route to prevent traumatising my boys and to not risking haemorrhaging again (as I lost a lot of blood during my first two births). Plus, the thought of going into labour and not having a baby at the end was so depressing that it simply wasn’t an option for me.
I was still hoping that only a little water had gone, so I refused to talk about it until I had my scan. I willed my baby to pull through and that my body wouldn’t fail on me. I kept drinking and must have gone through at least four litres of water in the last few hours.
15:00 – Friday 27th October 2017
I was finally ready to be taken to the scanning room, despite being told this would be at 9am, to find out whether my baby was fighting strong and that the copious amounts of water I drank had miraculously replenished my amniotic fluid.
Funnily enough (not funny), it was the same sonographer who did my 12-week scan, and she hadn’t been any more vocal than before.
I couldn’t see the baby and asked her why. She said it was because there was no amniotic fluid left.
I burst into tears. I knew what this meant. There was no saving my baby anymore.
I told her that was enough. I couldn’t be here anymore because there was no positive outcome. And in response, she turned up the sound of my baby’s heartbeat to show me she was still alive, but then told me that the pregnancy would have to be terminated because there was no chance I could replenish something that wasn’t there.
I thought to myself, is this how medical staff treat mothers who are facing the prospect of losing their babies? All I got was pure indifference and sheer negligence. I was so distraught and told her to turn the heartbeat off. I put my hand up to the screen so I couldn’t see my baby. I just couldn’t see her. The thought of having to kill her was too much and I willed her to rest in peace in my tummy instead if there was no other way to save her.
I cried into the midwife who accompanied me – she was so lovely and stayed with me throughout until I was reunited with my husband. I kept reading the different stories from mothers who PPROMMed full waters at 15 weeks and the stories were not positive. In fact, I read that those babies who were born later after a full PPROM would be seriously disabled and die from stillbirth anyway.
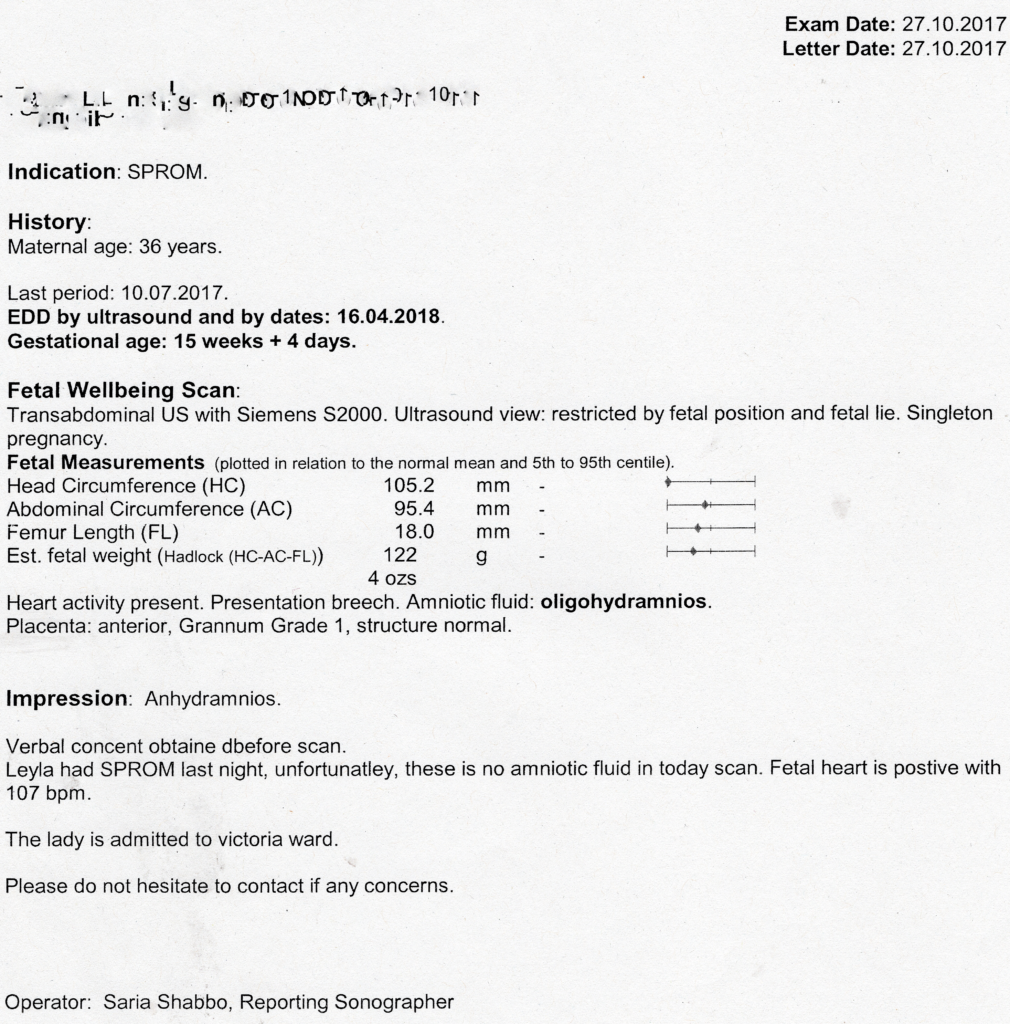
I was diagnosed officially with having a PPROM / oligohydramnios at 15 weeks pregnant and was provided with another two sets of antibiotics to prevent infection. My blood, urine and everything were checked and my baby kept moving as if to tell me she was still alive and there was hope still for us.
Yet medical staff around me was pushing me to go into natural labour because they didn’t think it was ethical to do a D&E. My hubby thought they were trying to free up the bed by offering a pessary to push things along. The whole time I kept hugging my baby.
And the whole time. I felt like a failure.
I failed my daughter.
18:10 – 27th October 2017
I was visited by another doctor to tell me the same thing again. There are complications with the surgery regarding removing the foetus and the bones splintering the womb.
18:30 – 27th October 2017
Again, another doctor came in to advise against medical surgery and that inducing labour was a safer option.
The treatment I had received throughout the weekend was shocking. I wasn’t allowed to go home to see my kids and that if I really wanted surgery, then I would have to wait until Monday, despite being warned that every day my ALIVE baby inside me was risking my health.
One of the junior doctors opined at how unethical it was to do a D&E because of the procedure and that I was better off letting labour take its course. When I mentioned to her, I had two boys at home who would be traumatised and that I had haemorrhaged during my last two births, her response was:
“Well, that’s an undesirable situation, isn’t it?”
That was it. Enough was enough.
For the first time since this entire ordeal began, I saw hubby lose his temper. The junior doctor cowered under his presence and ran off to get the surgeon.
20:00 – Friday 27th October 2017 to 08:00 – Saturday 28th October 2017
We were visited by a midwife after junior doctor after midwife at 20:00, then at 21:00, then at 22:00, then at 23:00.
02:00
04:00
06:00
06:30
08:00
They all asked. All checking to see if I had a temperature. All checking to see if I had changed my mind about the surgery.
10:45 – Saturday 28th October 2017
We officially complained.
There was no plan, no visit, no moving forward, nothing. Just doctor after doctor coming in and asking us the same questions. And all we got in response was apologies, and that the surgeon was very busy in the labour ward, but is aware of me and my situation.
11:15 – Saturday 28th October 2017
I was advised medical induction of labour again and that’s when I cracked.
“I don’t want a vaginal delivery! I want surgery, stop recommending it to me! I know my rights!”
12:50 – Saturday 28th October 2017
I was told that no one would do the surgery over the weekend and that they would have to defer me until Monday.
I was fed up and said I wanted to be discharged to go home. My baby was still holding on for dear life, I could feel her hugging me.
14:10 – Saturday 28th October 2017
I was finally discharged to go home and see my babies. It had been the longest time we were apart and as a result, my eldest was extremely anxious at seeing me. I later found out he thought I was dying with the baby, which still breaks my heart to this day.
After speaking to the top dog (Mister Rodin) who finally gave me the concern and attention that I deserved, he apologised for how long we had to wait to be seen by him. He had a few emergencies come up in surgery and he could not see us any sooner. He was one of the few doctors that could perform a D&E and that upon looking at my notes, this was the safest option because of the loss of blood observed in my last two births. A sideward glance from this wonderful doctor to the smarmy junior doctor provided us with a slither of justice.
He warned me there was no other way to keep the pregnancy and if my baby hadn’t gone to sleep before the surgery, he would have to inject her to help her go to sleep. I’m crying as I write this, but at the time I felt like waiting this long may have been a blessing because if my options were for her to go naturally or for me to kill her, I would have taken the former every time. But time was running out and the longer she stayed in my body, the longer both of us were suffering.
08:00 – Monday 30th October 2017
I was told to come back early on Monday morning to be the first on the list for surgery. But after waiting for a few hours in the reception room, hubby had heard the receptionist ask about where my notes were. It turned out that they couldn’t find my maternity notes and they had been missing since the weekend.
Plus, we were advised that there were no surgeries happening that day.
18:00 – Monday 30th October 2017
We were taken into a vacant room and bar being offered food, no one else visited us. At 6 pm a new doctor came in to tell me we had to go home and come back the next day when Mr Rodin would be available to perform the procedure. I had been nil by mouth since 12am that day so I was starving and extremely fed up. The doctor even had the audacity to advise that I should have attended a private clinic on Friday to do the procedure instead of waiting. I pointed out that Barnet Hospital had made me wait and didn’t advise this at all.
Hubby and I had McDonald’s and I stopped eating at 12am in anticipation of surgery the next morning.
We also mapped out our complaints procedure against Barnet Hospital and their rude and negligent staff.
Yet throughout all this, my baby was still moving but I could feel her getting slower and weaker. I knew my baby was on the way out, so I said goodbye to her before I slept and promised Poppy that I would never, ever forget her.
08:00 – Tuesday 31st October 2017
The next morning, we headed for surgery and I was given all the necessary medication to kick-start the surgery.
10:00 – Tuesday 31st October 2017
I was cramping and that’s when I felt my baby go. I don’t know how I knew or what made me feel like this, but I just knew she had finally gone to sleep and one last internal hug marked the end of my journey with Poppy. But I whispered to her she would always be my angel baby and that I was now a mother of three, just I wouldn’t be able to meet her in the flesh.
13:20 – 31 October 2017 – D&E Surgery – Goodbye Poppy
I woke up after vivid dreams of carving pumpkins with the boys and blinked at the flashing lights above me. For a moment, I had no idea where I was and I had forgotten all about what had happened before. Lights were being shone into my eyes, and I could hear beeping in the background.
A midwife welcomed me to the suite and asked me how I was.
“What happened?” I asked back.
“The surgery went well and we have your notes here. It states here you had a UTI and Group B strep.”
And with that statement, all thoughts of my Poppy came flooding back.
Poppy was gone.
I burst into tears.
“I have what?”
“It says here on your notes. But, please don’t be alarmed. I know you’re going through a lot. Group B Strep is very common during pregnancy. Around 40% of women have it.”
“Do you think this caused the PPROM?” I said through sniffles.
“I can’t answer that.”
“Because you don’t know?”
“Because Group B Strep can have adverse outcomes in pregnancy but it’s not causative.”
“So, you’re saying it didn’t cause it, but it may have been a factor? What about the UTI?”
“We can’t determine what may have caused your PPROM, I’m afraid, but we will refer you to a Bereavement Counsellor who can talk through with you about some options available for the funeral.”
I stared at the midwife in shock, then shook my head.
“Just go, please.”
I stared at the wall as the bereavement counsellor went through her script about how much support they’d offer me and that I had a choice about what I would like to do with my baby’s remains.
For five days I had begged for answers, got ignored, bullied into miscarrying naturally and being stared down rudely by oncoming staff because I was pacing up and down, stressed while waiting to go into surgery. Now I’m being asked what I would like to do with my baby’s remains, ten minutes after waking up from surgery, which hoovered my broken baby from my tummy.
I mean, really?
Shame on you, Barnet Hospital. Shame on you.
I thought long and hard about writing this article. I wrote to PALS who never wrote back. I left voicemail messages and got a call from someone a week later.
And guess what? Oh, yes, the good news just keeps on coming (!)
A year later, I was sent a letter from Barnet Hospital to inform me that my baby was buried in the communal funeral area, despite me checking the box AND telling the bereavement counsellor that I wanted to have tests done to find out what happened and to use her remains for further research.
All I say is, thank goodness I have kids to go home to because heaven help those poor first-time mums if they had to endure the same treatment and experience this kind of torture from a well-known North London hospital.
And, I’m not blaming the NHS – my mum works in NHS and not all hospitals are the same. Some hospitals, as you will find out in Part 4, are amazing.
But, Barnet Hospital was a nightmare, so much so, that if I decided to have another baby (hint, I did, but that’s for Part 4!) I would not touch Barnet Hospital with a barge pole.
First trimester loss, second trimester loss and third trimester loss are torturous and soul-destroying and you would expect to receive a standard level of care where you are treated as if you matter, even if staff are too busy. I understood and respected that the surgeon was helping others in worse positions than me. But to leave me in a room and offer no answers about my situation is unacceptable.
And, for that, three years later, I felt I had to write about it and share with the world, in case others had been treated in the same way.
It is not ok.
Post-surgery recovery
After the surgery, I felt numb. I had to go home and make Halloween treats for the boys so they could go out trick or treating. But I didn’t put a pumpkin out that year. I wanted to be alone and just stare into the void for a bit.
The following week we went for a very long walk in our neighbourhood park and hubby just let me walk on my own for a bit while he tended to the boys.
I felt empty most of the time, like I had lost a huge part of me.

The boys asked lots of question about Poppy and I had to break it to them they would never get to see her again, but she would still be their sister. My middle one, who was five at the time, amazed me by saying:
“It’s ok, mummy, as long as you’re ok, we’re ok.”
However, it hit my eldest (six) very hard and I saw him retreat inwards. His anxiety was exacerbated by the void he felt too, and he started to slip at school. My eldest was so heavily invested in looking after his sister, talking about her every day and planning how he was going to read to her. And now she was gone.
It then dawned on me that miscarriages don’t just affect the parents, they affect the whole family. And kids don’t understand why these things happen and so for them, it’s even worse. The boys thought they would meet their sister in April and now they aren’t. How do you explain to a five and six-year-old why that is?
During fireworks my son asked me if he could have just one present for his birthday.
“Of course. What would you like for your birthday?”
“Another sister.”
“New year, new start, ” I forced a smile through gritted teeth.
And, with that, I set about finding a way to live with the pain of losing my third child.


And every year, I light a candle for little Poppy during Baby Loss Awareness Week (9th to 15th October) and celebrate her birthday privately every 18th April. She would have turned four this year.
But, lighting a candle, helps me get through the pain of not being able to hold her as every mother should hold their babies but sometimes can’t.
And, now I realise that losing a child is the hardest pain to manage because it never ends. But we learn to live with it.
LetsGetChecked can help you understand your hormonal health with their female fertility testing options. Collect your sample from home and you'll receive accurate results within 2-5 days of the lab receiving your sample
Order now for 25% using the discount code MHD25*
Have you ever lost a child? How do you get through the day?
Some tips to managing baby loss
- Time makes it easier to manage the pain, but you will have down days. Have a strong support network around to pick you up during those days.
- It’s good to talk about it with someone close to you. Even if they have nothing to say, just venting helps the grieving process.
- Male partners deal with loss differently. If your partner gets through it by pretending your baby never existed, then don’t chastise them. Leave them to it to deal with it in their own way. Every person deals with grief differently. But stay united.
- First trimester miscarriages tend to be based on chromosomal abnormalities and second trimester miscarriages may be related to maternal infection. Neither miscarriage is your fault!
- Share your miscarriage story with us at Motherhood Diaries to stop this subject being taboo. Miscarriage is unfortunately extremely common, with 1 in 4 experiencing a miscarriage. It’s even rarer to experience 2nd trimester miscarriage, with 1-2 out of every 100 experiencing a late miscarriage. So, we need to share with other women that we’re there for them and we support each other through these horrible times.
- It’s hard to spot the signs of miscarriage in the second trimester, but if you are worried about anything during your pregnancy, whether that be abdominal cramping or spotting, visit your GP straight away, even if it’s a minor ailment.
- Try to stay away from Google when you’re searching for answers. The conflicting information will frustrate and overwhelm you.
- But join Facebook groups for the support. If I hadn’t confided in the Facebook groups I joined I would have felt much, much more alone. It’s a group we never want to join, but it’s one of the most welcoming and supportive if you, unfortunately, end up having to do so.
If you would like to share your first or second trimester miscarriage and stillbirth stories on Motherhood Diaries, please click on the link here to access the form. The more we share, the more we support each other, especially during Infant Loss Awareness Month, Baby Loss Awareness Week and World Mental Health Day which is today.
I joined Birmingham Women’s Hospital to #Take10At10 to support those affected by baby loss and the creation of Woodland House, a standalone bereavement centre that will help so many families:
Join us on social media via Facebook, Twitter, LinkedIn and Instagram now and #Take10at10 too.
What happens next?
On 20th February 2018, I emailed Dr. Verma to tell him I was ready to try again and you can read all about my journey to getting my girl in Part 4 here.
Thanks for reading.
*Links marked with a ‘*’ are affiliate links which means I may earn a small commission on qualifying purchases








3 Comments