Amelia’s Unassisted VBAC Story
What a crazy experience!
I could not have foreseen how it all started and how it ended with my fourth and final baby.
I will preface this unassisted VBAC story by saying that I did everything to encourage my baby out naturally. I followed all the natural birth induction techniques and I pushed the scheduled Caesarean for 41 weeks to 41+5, but baby had no interest in coming out yet.
Getting ready for my C section
The night before my C section, I didn’t eat or drink anything from 10 pm and took the offered two omeprazole to reduce my stomach acidity before the operation. I woke up at 5 am after a vivid dream of missing my C section (I was secretly miffed that I hadn’t actually missed it). Surprisingly, all three kids had woken up too. They must have sensed what was to happen today and my frayed nerves.
I took my second two tablets at 6 am with my last sip of water and called Watford Hospital to confirm the time to come in, which we were told was 7 am. We dropped the kids at the grandparents’ and headed to the Katherine Ward at 7.10 am where we were asked to complete a Covid PCR test for me and a lateral flow test for hubby. Thankfully, the results were negative, so we could continue with our baby journey.
Instead of a C section, why not try this new induction method?
I was starving as I had been nil by mouth since 10 pm, yet hubby was busy munching away on the snacks he bought me for post-surgery. A consultant doctor came to see me while I waited on a hospital bed that had a nightgown and compression socks sitting patiently on top in anticipation of the surgery. The doctor must have spied the sheer horror on my face after she confirmed I was scheduled for a c section because she asked whether I had been offered a new type of induction that involves Dilapan and is safe for previous c section patients. The new induction doesn’t involve the hormonal drip syntocinon so it doesn’t cause artificial labour and place unnecessary risk on uterine scars.
I replied I hadn’t but had no idea what this new induction process was. She explained that Dilapan works by placing rods inside to soften and open the cervix enough to break the waters. She hoped the process would stir my baby enough to incite contractions. They also offered an epidural during the procedure, which I happily accepted. You don’t get a medal for taking labour pain!
We had to wait three hours in the Katherine Ward until we were taken to the Victoria Ward where I could stay in a private room. Hubby had to leave at this point and could only return once I was in active labour. And who knows when that was going to happen, seeing as I had only felt tightenings at this point.
I was offered a lunch menu, but there was more waiting around. I mentioned I was to be prepped as GBS positive, which wasn’t stated previously by any other doctor. I had to mention again to be sure because I had heard a horrible story recently that a mother’s newborn baby had died from contracting Group B Strep and as I was tested positive during my miscarriage in 2017 and was treated for antibiotics in 2019 with my third pregnancy, I didn’t want to risk this little lady.
At around 10.30 am a lovely woman in purple overalls, Angelica explained the Dilapan process again, i.e. they will insert rods into my cervix and there shouldn’t be any pain. Then when labour starts or I get contractions, I will be asked if I want an epidural before my waters are broken and I will then be placed on IV meds for Group B Strep. She warned that the induction process could take up to 12 hours to work. So they would monitor baby first for half an hour then they would start the induction process. It was just a waiting game now. It could still end in caesarean but at least I was giving VBAC another good shot.

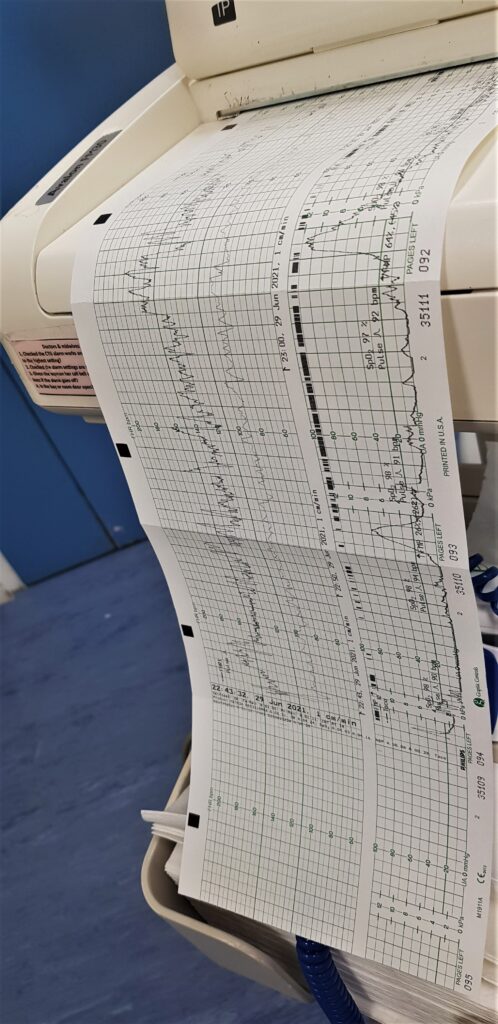
So they hooked me up to the CTG for thirty minutes to check if baby was still ok. The heart accelerations which I was told was how it should be for babies was between 120 to 167. Every time I had a tightening, baby’s heart rate would go up slightly then dip, which apparently was normal. But she kept moving around so the heart rate would disappear off the screen. During the monitoring, one of the staff members brought over some lunch; jacket potato with cheese, banana and apple juice. Unfortunately, I couldn’t eat as I was hooked up to the monitor and lying on my side.
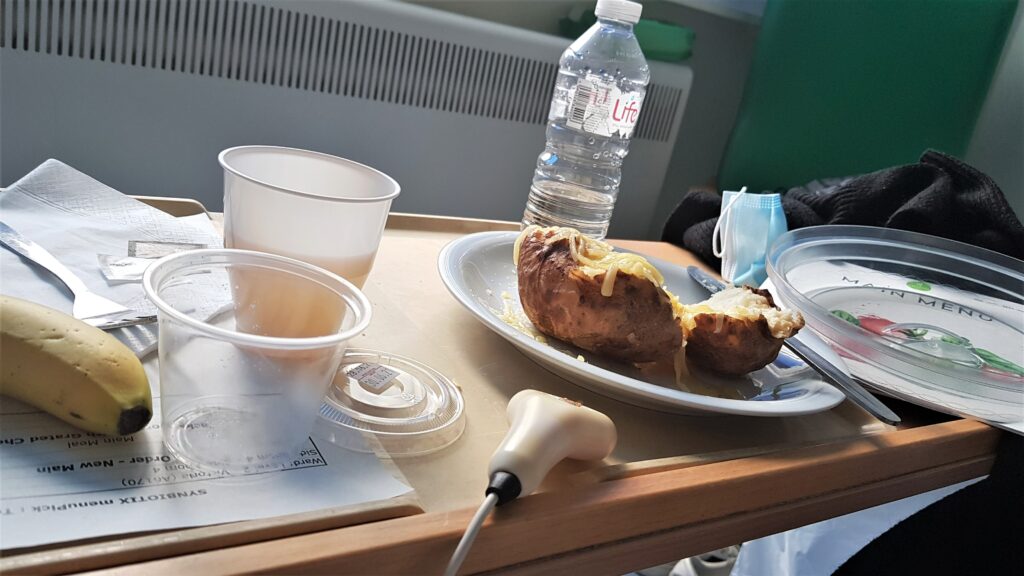
After about an hour, I was told I could change position to lie on my back so I could eat lunch. Before 2 pm, I was taken off the monitor to wait for the induction process that was just next door. Once the induction process was over, I’d come back and be placed back on the monitor to gauge if baby was happy with it all.

I was annoyed that hubby couldn’t be around until active labour. I found it hypocritical that 15,000 people could go to Wimbledon or 60,000 people could watch the Euros but my hubby who tested negative from the lateral flow test couldn’t be with me at hospital. I get that it is a hospital environment with vulnerable newborn babies so it’s better to be extra careful. However, I believe a lot of the decisions made by the government are economic and contradictory. Anyway, I’ll move past the politics!
There was more waiting around and at 2.30 pm I was called next door to have the Dilapan fitted. The rods looked long and scary and I was worried it would be uncomfortable when inserted (they would insert up to five rods). I had to take my bottoms off and place my legs on the stirrups. The lovely doctor inserted some jelly to check my cervix and good news! She said I didn’t need the induction because my cervix was quite open and baby was very low. So now all was needed was for them to break my waters to ramp up labour.
She tickled baby’s head a bit to spur baby on but they couldn’t break my waters yet because it could trigger labour rapidly and they didn’t have the equipment available at the floor we were on. But I had to wait to break the waters because more important women were going ahead of me. I just hope this baby could hold on for a while longer before they called time on the waiting and brought me to theatre for the c section.
At 4.30 I was still waiting, so I got out my laptop and started working. I actually got a lot of work done, the wait was so long!
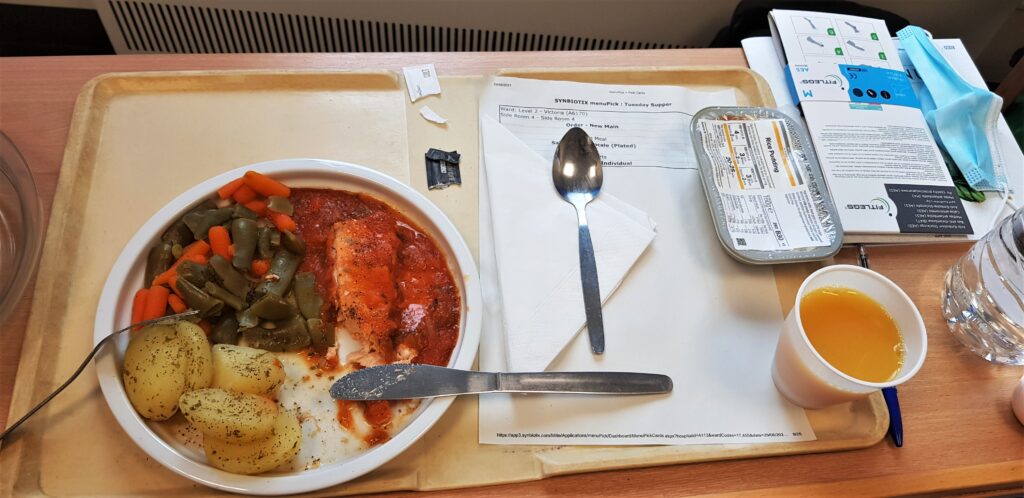
At just before 6 pm, I had my dinner; a salmon Provencale and rice pudding with an orange juice. I watched many episodes of Firefly Lane and even finished the series!
My mum who works at Watford Hospital, asked to visit but only partners could be present during designated visiting hours, despite hubby not being allowed to come in until labour. I was so bored, I tried to work but I just wanted this baby to greet me with her presence. I wanted the hospital to call me to break my waters and it even crossed my mind that it may have been better to go through with the elective c section because at least I would have had my baby by now!
At 7.30 pm a student midwife called Eleanor came to do my obs again (blood pressure and body temperature). She told me that 22 mums were delivering, but they were trying to get a constant update for me. There was good news though; baby was slowly turning back to the front-to-back position, which is an optimal position for labour, so I was hopeful she was doing her thing in time for birth. Baby’s heart rate was also checked and it was fine, although the midwives warned me there won’t be any movement until after the shift change tonight, whenever that was going to be.
Hubby could visit between 6 and 8 pm but he wasn’t able to come anyway because he had to retrieve the other three kids from the grandparents as they were exhausted. So I told him to stay with them until I had more updates or at least until my water broke, whenever that was going to be as it was now 8 pm!
At 8.40 pm there was a shift change and one midwife informed me it was very busy upstairs in the delivery suite. I was placed in a queue with up to four other women, and I was last in that queue, even though we were all at differing levels of riskiness. I realised it was highly unlikely my baby girl would come that night, so midwives advised they would do another set of obs at 10 pm to check whether baby was still happy but that was about it.
At just after 10 pm, the midwife came to do the CTG and baby’s heart rate was still between 120 and 170 so she was still happy. The CTG didn’t come off until 11.35 pm, however, so I was encouraged to sleep and they’d wake me if there was any movement in going upstairs to break my waters.
At 2 am, baby and I were monitored again. All was still fine except I couldn’t sleep because the bed was so uncomfortable. And when I slept, I woke up throughout the night because of painful tightenings. I got myself up properly at 5.30 am because the pressure down below was too strong to sleep through. Could this be labour starting?

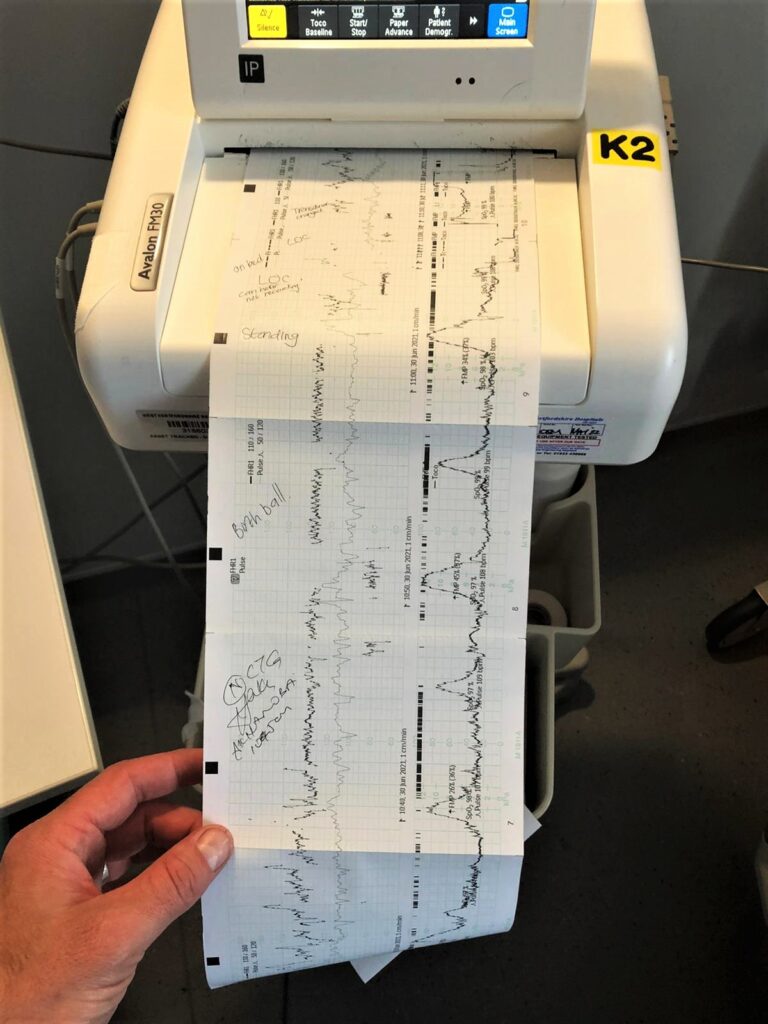
I was monitored again and could see the contractions had started, but they were irregular. I was hooked to the CTG for a long while but finally I was called upstairs at around 10 am and was taken to the delivery suite. A lovely positive woman called Corina hooked me up to another CTG and she also gave me a birthing ball to bounce on to help baby move down. It was a lovely room with a flat-screen showing the CTG movements.
The VBAC story begins
Hubby finally made his appearance, for which I was grateful and soon after the midwife examined me.
I was at 6cm!
I was shocked. The contractions were still manageable and not at all bad like last time. The midwife said it was because the baby had turned from Occiput Posterior (back to back) to transverse (side) position and she was slowly turning front to back which was the optimal position for labour and birth. Even being transverse made such a difference with the pain as it wasn’t centred in my back like last time, which had been excruciating.
Corina broke my waters, which was uncomfortable because there was so much tugging involved and then what happened in the next 15 minutes was a blur.
I started on gas and air (Entonox) somewhere between 7 and 8cm and around five minutes later the contractions had ramped up so hard that hubby said I sounded like a wolf and an owl at the same time. The pain was unbelievably strong. I cried for pain relief and they said the anaesthetist had been called but she never came.
Suddenly I had an urge to push, like the need to go to the toilet. I just remember the midwives telling me to listen to my body but it was very much like needing to go for a massive poo! You can’t control it.
Corina told me to breathe slowly to avoid tearing, and then she told me to give it one last massive push. I kept shouting that I couldn’t do it. I was so tired and the pain was so horrible, but she told me I was doing it and to keep going. I remember the stinging and I thought at that moment I must have torn. One big crazy push and I felt the biggest relief, like a massive pop and it was euphoric.
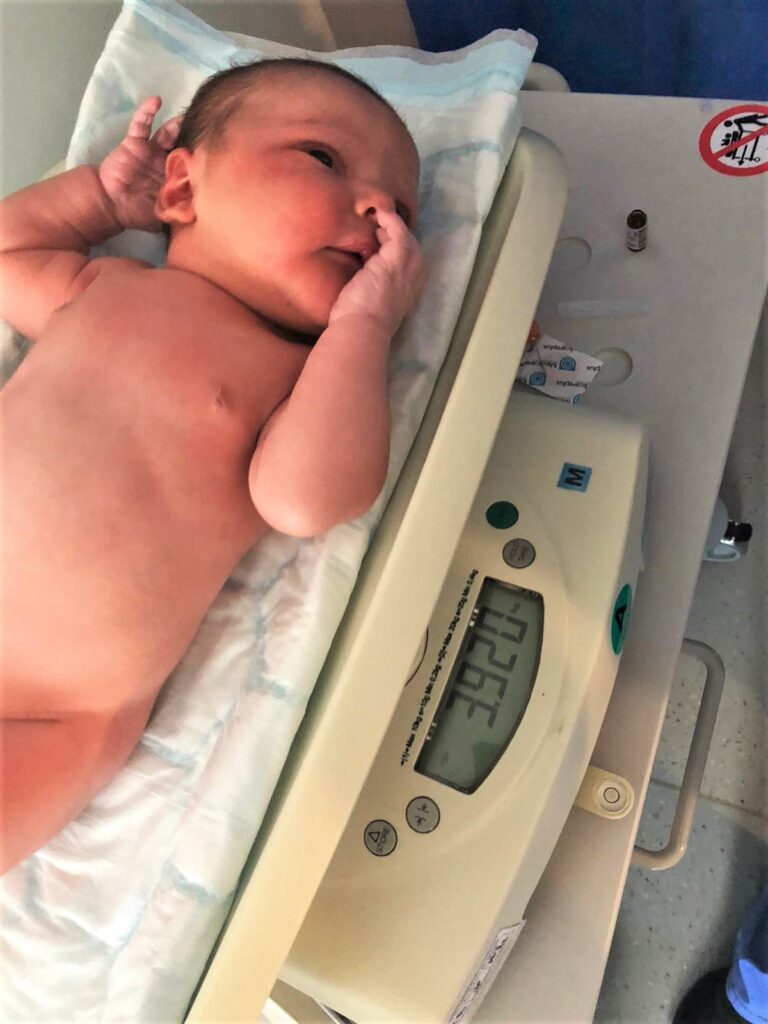
Baby girl Amelia was out at 13.56, which meant that I had laboured for just under four hours and pushed her out within 15 minutes! Amelia weighed a massive 3.920kg / 8lbs 9oz and I had no pain relief except for gas and air.
What!?


Amelia chilled on my chest and rooted for milk. She attached beautifully, but her nose was blocked so she struggled a bit to breathe in while she was feeding. The midwives said she had received quite a shock flying out of the birth canal so quickly. So she had to be resuscitated, but once we heard that cry it was joyful and I felt so proud of myself and Amelia for helping each other get through the birth. Apparently, hubby said Amelia was moving around a lot to get into the right position, which I think helped with the shorter labour.

Pushing the placenta out was interesting too. I had to do another big push although it wasn’t as painful as birthing the baby. The placenta came out a few minutes later.
The nurses checked me over downstairs, which I needed gas and air for because it stung so much, but they only found grazes, which meant no stitches too.
Double what!?
I went from coming in to be prepped for a c section to pushing my baby out without pain relief in 15 minutes and needing no stitches! The pain was ridiculous. The pushing is even crazier but once you push your baby out, the feeling you get is nothing short of amazing. I am so glad they turned the epidural away. I could walk around post-birth, albeit with a bit of stinging. I could stay mobile. I had no drugs coming through my system after having a medication free birth and it felt amazing. What a positive VBAC birth story of a big baby weighing almost 9lbs too!

We stayed in the recovery suite until around 6 pm where hubby ordered a Burger King post-birth meal which tasted sublime. I also had toast and a lovely cup of tea which were delicious.


I was then wheeled to the postnatal ward with Amelia in my arms. There were four other women at the ward all with different birth stories but it was lovely to chat with them and share their birth experiences. The bleeding was uncomfortable as it’s baking at the hospital and the beds aren’t particularly comfortable.

No one told me about the afterpains, especially after four kids! Every time I breastfed, my uterus contracted and it felt like a mini contraction, I needed painkillers! Apparently, it takes longer for the uterus to contract back down to size after it has swelled like a balloon four times. Breastfeeding was proving quite difficult because of Amelia’s blocked nose, but the midwives said she was slowly clearing it herself, so it was better to leave it but they offered saline drops in case breastfeeding was becoming a problem.

As a result, it became painful to breastfeed but I noticed it was slowly getting better, so I persevered.
As I wasn’t allowed visitors, I was desperate to see my family and show off baby Amelia. I was advised I would be discharged the next day which was great because I thought I’d be here for three days and neither of us slept well the first night that I doused myself in sugar to stay awake. Amelia was completely clogged up, but thankfully she passed the hearing test at around 10.30 am the next morning and the newborn check.

Her nose slowly cleared by the afternoon and she had a nice long nap in bed.

I was discharged to just midwifery care in the afternoon so I just had to wait for the go-ahead and we were ready to go home! I was prescribed Enoxaparin, which is blood-thinning medicine to prevent thrombosis (blood clots); I showed two risk factors, which were my age and the number of kids I’ve had.

At around 5 pm hubby came to pick me up and I was shocked that I was able to walk so easily back to the car, which was a wonderful experience, even though my hips and front bottom felt sore and I was tired from not sleeping well the last few nights.


What an amazing experience and it goes to show you never know what’s around the corner! Thank you so much to two wonderful midwives, Corinna and Lucy. They were paramount in helping me achieve the most perfect VBAC birth story after three very different birth experiences. I can’t believe I managed another vaginal birth after two caesareans!


My VBAC experience was perfect for me. But, I learned that everyone’s perfect birth is different and as long as it is a positive one then it’s perfect for you and baby.

Click here for more beautiful birth stories (including home birth and caesarean) and for my other birth experiences please visit my Birth Diaries page here.
You can buy the Snuzpod 4 here and Save Up To £53 with SnuzPod4 Bedside Crib Bundles*
Need to know your pregnancy due date? We have a calculator for you right here!
FAQ
Am I a good candidate for VBAC TOLAC if I had my first child by cesarean 12 years ago? My firstborn was a breech birth?
Whether you are a good candidate for a trial of labour after caesarean (TOLAC) or VBAC depends on several factors, including your specific medical history and current circumstances. It’s best to consult with your doctor to assess your individual situation and determine whether VBAC is suitable for you.
In general, having had a previous caesarean section, especially for a non-recurring reason such as breech presentation, does not automatically exclude you from being a candidate for VBAC. However, other factors will need to be considered, including:
- Breech presentation is not a recurring indication for caesarean section. The reason for your previous caesarean may have an impact on your eligibility for VBAC. For example, if the caesarean was performed due to a specific condition that could recur or if there were complications during the previous birth, it may affect the recommendation for VBAC.
- The type of incision made during your previous caesarean can influence the feasibility and safety of a VBAC. A low transverse incision (horizontal incision) is generally considered more favourable for VBAC compared to other types of incisions, such as a classical vertical incision.
- The length of time since your previous caesarean can impact the likelihood of a successful VBAC. A longer interval, such as 12 years in your case, may be associated with a higher chance of VBAC success. For more VBAC success stories, you should Google ‘vbac success stories forum’ or ‘vbac experience forum’ to read other success stories.
- Your overall health, current pregnancy, and any new complications or conditions need to be taken into consideration. Factors such as the size and position of the baby, any placental issues, or other medical conditions may influence the recommendation for VBAC.
- The availability of immediate emergency care, including an operating room and a skilled surgical team, is important in case of any unforeseen complications during a VBAC attempt.
Attempting VBAC Vaginal Birth after Cesarean. What can go wrong? Can pushing rupture previous stitches in the ovaries? What is the recourse in that condition?
Attempting a VBAC carries certain risks, and it’s important to be aware of them. While VBAC can be a safe option for many women, there are potential complications, which you should discuss with your healthcare provider to make an informed decision.
Some potential risks and complications associated with VBAC include:
- Uterine rupture, which is the most significant concern with VBAC. Uterine rupture is a rare but serious complication where the scar from the previous C-section tears during labour. It can result in severe bleeding and pose risks to both the mother and baby. Emergency surgery, such as a C-section, is typically needed if a uterine rupture occurs.
- Any type of delivery carries a risk of infection. However, the risk may be slightly increased in VBAC due to extended labour and multiple vaginal examinations.
- There is a possibility that VBAC may not be successful, and a C-section may still be required. Factors such as labour progression, foetal distress, or other complications can lead to a change in plans.
Regarding your specific concern about pushing rupturing previous stitches in the ovaries, it’s important to note that the ovaries are not typically involved in the uterine incision made during a C-section. C-section incisions are usually made on the lower segment of the uterus, away from the ovaries. However, it’s always best to discuss any specific concerns related to your previous surgery with your doctor.
In the event of a complication during a VBAC, such as uterine rupture or other emergencies, the medical team will be prepared to provide immediate medical intervention. This may involve performing an emergency C-section, providing blood transfusions if necessary, or taking any other appropriate measures to ensure the safety of both you and baby.
What happens if you refuse a C section in a hospital that has a VBAC ban but won’t travel to a different hospital? Do they still have to admit you?
The policies regarding VBAC and C-sections can vary between hospitals and healthcare providers. If a hospital has a VBAC ban or a policy that restricts VBACs, it means that they may not offer VBAC as an option for childbirth.
If you refuse a recommended C-section in a hospital with a VBAC ban but are unable or unwilling to travel to a different hospital, the hospital may still have a responsibility to provide you with appropriate care. However, it’s important to note that this depends on the hospita’s policy.
Have an open and honest conversation with your healthcare provider about your concerns. They may be able to provide other options that prioritise your health and well-being while respecting the hospital’s policies.
In some cases, it may be possible to talk to other healthcare professionals, such as obstetricians or midwives, who have experience with VBAC and can provide additional guidance.
You must be proactive in advocating for your own care and seek information about your rights and within the healthcare system in your country or region. Consulting with a patient advocate or seeking legal advice, if necessary, can help you understand your rights and potential courses of action in situations where you and your healthcare provider may have differing views on the best approach to your care.
Can you have a successful VBAC after 3 c-sections?
Other questins asked were:
- Can you have a successful VBAC after 4 c-sections?
Having a successful vaginal birth after three previous caesarean sections (VBAC3) is possible in some cases, but it generally carries higher risks and is considered more challenging compared to VBAC after one or two previous caesarean sections. The decision to attempt a VBAC after three C-sections is complex and should be made in close consultation with a healthcare provider experienced in managing high-risk pregnancies.
Factors that may influence the possibility of a successful VBAC after three C-sections include:
- The type of uterine incisions from the previous C-sections can impact the safety and feasibility of a VBAC. Ideally, low transverse incisions (horizontal incisions) are preferred for VBAC as they have a lower risk of uterine rupture compared to other types of incisions, such as classical vertical incisions.
- The doctor will evaluate the healing of the uterine incisions from the previous C-sections. If there are concerns about the integrity or strength of the uterine scar tissue, a VBAC may not be recommended due to the increased risk of uterine rupture.
- Other considerations include your overall health, any additional medical conditions, the size and position of the baby, and the availability of emergency resources in case of complications during labour.
Given the complexity of your situation, it is crucial to consult with a healthcare provider experienced in managing high-risk pregnancies and VBAC after multiple C-sections. They will be able to provide you with peronalised advice based on your specific medical history, conduct a thorough evaluation, and discuss the potential risks and benefits associated with attempting a VBAC after three previous C-sections.
Would you mind sharing your successful VBAC story after having an emergency C section?
This is my birth journey as I didn’t have a VBAC after an emergency C section. I hope it helps:
- 2010 – First pregnancy – Emergency C Section birth experience here
- 2012 – Second pregnancy – Planned C Section story here
- 2019 – Third pregnancy – Assisted VBAC story here
- 2021 – Fourth pregnancy – Unassisted VBAC (which you can read above!)
What should I do to have a successful VBAC?
Other questions asked were:
- Are you a good candidate for VBAC?
- Ways to prep physically for VBAC?
To increase your chances of having a successful VBAC, here are some general recommendations:
- Look for a healthcare provider who is experienced and supportive of VBAC. They should be knowledgeable about the latest research and have a positive attitude towards VBAC. Consider discussing your intentions with different providers to find the one who best aligns with your goals.
- Discuss the details of your previous C-section with your healthcare provider. Factors such as the type of uterine incision and the reason for the C-section can influence the feasibility of a VBAC. Understanding the specifics of your previous birth can help you make an informed decision and determine if VBAC is a suitable option for you.
- Enrol in childbirth education classes that specifically cover VBAC. These classes can provide valuable information about the process, techniques for managing labour pain, relaxation methods, and coping strategies. They can also help you feel more confident and empowered in your decision.
- Prioritise your health and well-being during pregnancy. Eat a nutritious diet, engage in regular physical activity (as advised by your healthcare provider), and attend prenatal check-ups to monitor your progress. Staying healthy can contribute to a smoother labour and delivery.
- Learn about the stages of labour, various birthing positions, pain management options, and potential interventions.
- Surround yourself with a supportive network of family, friends, or a doula who can provide emotional support during your VBAC journey.
- Openly communicate your desires, concerns, and expectations with your healthcare provider. Ensure that your birth plan clearly outlines your intentions for a VBAC and any specific preferences you may have during labour and delivery.
Would a VBAC be better than a second c section?
The decision between a vaginal birth after caesarean (VBAC) and having a caesarean a second time depends on various factors and you should discuss these factors with your doctor. Both options have their own advantages and potential risks, so it’s important to consider individual circumstances and preferences.
VBAC can be an appropriate choice for many women. Some potential benefits of VBAC include:
- VBAC avoids the risks associated with surgery and the recovery time needed after a C-section.
- After a vaginal birth, the recovery time is usually shorter compared to a C-section, allowing you to resume normal activities more quickly.
- VBAC generally carries a lower risk of infection, bleeding, blood clots, and damage to internal organs compared to a C-section.
However, VBAC is not without its risks and limitations. Some factors that may affect the feasibility of a VBAC include:
- The type and location of the uterine scar from the previous C-section can impact the safety of a VBAC. A low-transverse incision (horizontal incision) carries a lower risk of uterine rupture during VBAC compared to other types of incisions.
- Certain medical conditions or complications during pregnancy may increase the risks associated with a VBAC, and your healthcare provider will consider these factors when making a recommendation.
- VBAC is generally considered safer when there is prompt access to emergency medical care, including an operating room and an experienced surgical team, in case complications arise.
What is a VBAC water birth?
A VBAC water birth refers to the combination of a vaginal birth after caesarean (VBAC) and giving birth in a water birth setting. It involves labouring and delivering the baby in a pool or tub of warm water. While VBAC itself refers to the mode of delivery, water birth is a birthing method that provides pain relief and a soothing environment during labour and delivery.
Water birth is a natural childbirth method that has gained popularity in recent years. Many women find it helpful for pain management, relaxation, and promoting a sense of calmness during labour. The warm water can help to ease muscle tension and provide buoyancy, which may make contractions more manageable.
When considering a VBAC water birth, it’s essential to discuss the option with your healthcare provider, as it may depend on various factors. Some factors to consider include:
- Not all women who have had a previous C-section are considered good candidates for VBAC. The safety of VBAC depends on factors such as the type of uterine scar from the previous C-section and the overall health of the mother and baby.
- Water birth may not be available in all hospitals or birthing centres. It’s important to check if the facility you plan to give birth in offers water birth options and whether they allow VBAC in a water birth setting.
- Some hospitals may have specific policies or guidelines regarding VBAC water births. It’s really important to discuss your and preferences with your doctor and ensure they are supportive and knowledgeable about this birthing method.
- Each pregnancy and birth situation is unique, and certain conditions or complications may make a VBAC water birth unsuitable. Your doctor will evaluate your specific circumstances and help you make an informed decision.
How long can you push in labour before c section?
In the UK, the duration of pushing during labour before considering a caesarean section (C-section) can vary depending on several factors. The decision for a C-section is typically based on the individual circumstances and the well-being of both the mother and baby. The duration of pushing alone may not be the sole determining factor.
In the UK, healthcare providers generally follow guidelines provided by the National Institute for Health and Care Excellence (NICE) when making decisions about childbirth. However, it’s important to note that specific practices and policies may vary between healthcare providers and individual cases.
According to NICE guidelines, if a woman is having a vaginal birth, the second stage of labour (the pushing stage) should usually be actively managed if progress is not made within two hours. However, this time frame can be extended to three hours for women who have previously given birth and to four hours if regional anaesthesia (such as an epidural) has been administered.
These guidelines are not set in stone and healthcare professionals will take into account various factors, including the well-being of the mother and baby, the progress of labour, and the overall clinical situation. They will make an individualised assessment and determine the most appropriate course of action, which may involve a C-section if necessary.
Ultimately, the decision regarding the timing of a C-section during labour is a complex one and is based on the judgement and expertise of the healthcare provider, taking into consideration the specific circumstances of each case. It’s recommended to discuss any concerns or questions you have about pushing and the potential need for a C-section with your doctor.
Do you have any real VBAC stories to inform/inspire your birth journey?
Yes I do have some VBAC birth stories for you! Please checkout some success VBAC stories here. VBAC NATURAL BIRTH STORIES
You can find my hypnobirthing VBAC story here too: HYPNOBIRTHING SERIES
Why do doctors discourage VBAC?
Other questions asked were:
- Why do hospitals ban VBAC?
While it is not accurate to say that doctors universally discourage a VBAC, some hospitals may approach a VBAC with caution or discuss the risks associated with it. Here are a few reasons why some doctors may be cautious about VBAC:
- The primary concern associated with VBAC is the risk of uterine rupture, which is when the scar from a previous C-section tears during labour. Although the risk is relatively low, uterine rupture can be a serious and potentially life-threatening complication for both the mother and baby. Doctors may weigh this risk against the potential benefits of VBAC.
- VBAC is considered safer when there is immediate access to emergency medical interventions, including an operating room and a skilled surgical team, in case complications arise. Some hospitals or birth centres may not have the necessary resources readily available, which could influence a healthcare provider’s recommendation regarding VBAC.
- The type and location of the uterine scar from a previous C-section can impact the safety of VBAC. A low-transverse incision (horizontal incision) carries a lower risk of uterine rupture compared to other types of incisions, such as a vertical incision.
- Certain maternal or foetal conditions or complications during pregnancy may increase the risks associated with VBAC. Factors such as a history of multiple previous C-sections, a large baby, placental complications, or certain medical conditions may influence a healthcare provider’s recommendation.
- In some regions, hospitals may have concerns about the potential legal implications associated with VBAC due to the risk of complications or adverse outcomes. These concerns can influence their approach to discussing VBAC with their patients.
What is the failure rate of VBAC?
Other questions asked were:
- What are VBAC Pros and Cons?
- Why is VBAC controversial?
- What are the risks of having a VBAC?
There is no universally fixed failure rate for VBAC, as it depends on individual circumstances and the specific criteria used to define success or failure.
In the UK, the success rate of VBAC is generally reported to be around 70-75%. This means that approximately 70-75% of women who attempt a VBAC are successful in giving birth vaginally.
In the US, the success rate of VBAC is slightly lower, ranging from 60-80%. The success rate can be influenced by factors such as the type of uterine incision from the previous C-section, the reason for the previous C-section, the mother’s health, the size and position of the baby, and other individual factors.
It’s important to remember that success rates can vary between different healthcare settings, healthcare providers, and individual cases. Some factors that can affect the success of VBAC include the type of uterine scar, the experience and expertise of the healthcare team, access to emergency care, and the presence of any underlying health conditions.
*Affiliate link










One Comment