Why growth scans are important in pregnancy
*Motherhood Diaries worked with MyBaby4D in Watford (Ultrasound Image Studio Ltd) to raise awareness among pregnant couples about the importance of ultrasound scans during pregnancy to monitor the health and well-being of your baby. We were provided with the opportunity to review the Growth & Presentation Scan for the article – all opinions are 100% my own*
During your pregnancy, you should have routine scans via the NHS at around 12 weeks (nuchal translucency scan or dating scan) and 20 weeks (mid-pregnancy or anomaly scan). In this MyBaby4D Pregnancy Scan Series, I’ve talked about the importance of early scans (before 12 weeks) and wellbeing scans (from 16 weeks), which can provide that extra bit of comfort that the baby is doing OK, as there is a lot of time in between each NHS scan. Unfortunately, we don’t have a camera inside our uterus.
If necessary, you may be offered a foetal Growth scan between 28 and 40 weeks, too. We will discuss growth scans in more detail in this article.
Why are growth scans necessary?
I wasn’t aware of growth scans until my second baby measured big for dates (my bump was slightly bigger than the estimated week of pregnancy). So, I was scheduled to go for a foetal growth scan at 36 weeks to see if he was measuring slightly on the larger side and if there were any indicators of increased amniotic fluid (more on this below) and gestational diabetes. Otherwise, I would have no idea growth scans existed.
In recent years, hospitals’ focus has been on stillbirth prevention, as stillbirth rates in the UK were among the highest in Western Europe and had not changed much over the last twenty years. Most stillbirths were classed as ‘unexplained’, which meant these deaths were unavoidable. However, independent case reviews have been conducted to find that many stillbirths were associated with substandard antenatal care and, therefore, potentially avoidable. Most stillbirths showed that there was growth restriction during pregnancy, which had not been recognised during antenatal care. This meant that most women never had a growth scan, therefore there was no special attention until there was an absence of foetal movements, which was usually when it was too late.
Therefore, a better classification system came about that included categories for foetal growth restrictions (e.g., small for gestational age, which is a factor that increases stillbirth sevenfold). This report also found that recognising foetal growth restriction during antenatal care can halve the risk of stillbirth if discovered early.
The RCOG guidelines developed an algorithm that set out the recommended assessment of early pregnancy risk factors and the route of care for low-risk and high-risk pregnancies with foetal growth restriction. Those with an increased risk would require a growth scan and assessment. However, this was found by many hospitals to be too complicated, so The Journal of British Medical Ultrasound Society, Ultrasound, helped the NHS develop a simplified algorithm that identified a list of risk factors as part of the Saving Babies’ Lives Care Bundle initiative. You can find more information on these risk factors in the image below:

Growth scans in the NHS
The NHS now prescribes routine growth scans until delivery for those considered high-risk between 28 and 40 weeks.
Our growth scan at MyBaby4d Watford – 30+2 weeks
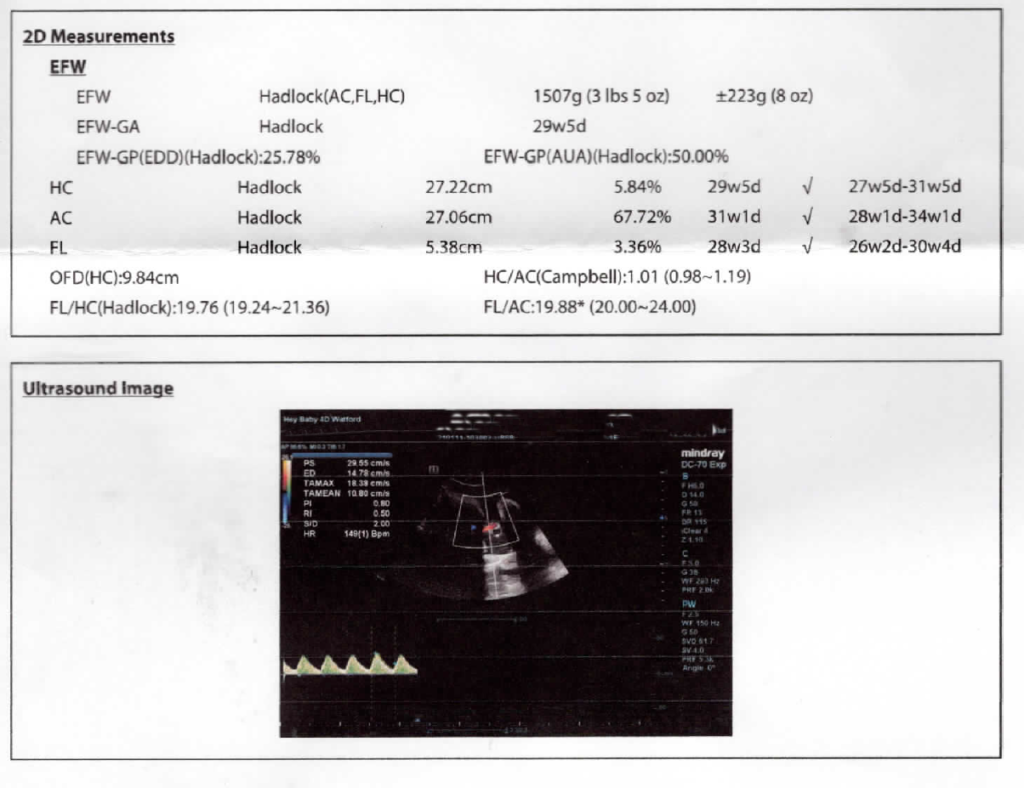
I attended a private Growth & Presentation Scan at 30+2 weeks with MyBaby4D in Watford, a 15-minute appointment to check the baby’s wellbeing, heartbeat, movement, weight and measurements. The primary objective of the third-trimester growth scan is to check the well-being of the baby, so I will go through each aspect of the foetal Growth Ultrasound scan taken by Dalson, the sonographer and break down each part below to show what happens at a Growth scan during pregnancy.
Preliminary questions
Dalson asked if I had had a growth scan before, if the NHS mentioned having one at 36 weeks, and whether I could notice a pattern in the baby’s movements. I told her this baby doesn’t really move much; she just shifts from side to side. But during the scan, she was dancing away, and I did wonder whether the ultrasound waves were too loud for her.
“Fetuses can hear ultrasound and the sound is as loud as a subway train entering a station.”
[Obstetrical ultrasound: can the fetus hear the wave and feel the heat?] [Article in German] J S Abramowicz et al. Ultraschall Med. 2012 Jun.
I also find that the baby moves more when I’m on my back. I often wonder whether I’m squashing her in that position and whether that’s why we are advised to lie on our left side while sleeping and napping. Lying on your right side puts pressure on your liver, so the left side is optimal.
During the scan, Dalson checked the following:
The head
We saw a bird’s-eye view of the baby’s head, and Dalson measured the head circumference. Dalson confirmed that the baby’s head was down, but she did state that the baby could still move at this stage. Until 34 weeks, they can still turn, but generally, babies may settle in a head-down position around 32 to 36 weeks. The baby’s head measured within the normal range.
Legs and Feet
We saw the baby’s legs stretched out, and the feet, too. Dalson struggled to measure the thigh bone as the baby’s hands on her bottom caused shadowing. I was asked to move to the side as our girl was kicking and munching away on amniotic fluid.
Amniotic Fluid Index
Dalson measured the single deepest pocket of fluid for the Amniotic Fluid Index, which should be between 2 and 8cm. Too little fluid means oligohydramnios (which is what I saw in my third ultrasound scan during my second-trimester miscarriage when I broke my waters at 15 weeks) or polyhydramnios. I was measuring at 7.7cm at the top of the normal range. Dalson mentioned that at MyBaby4D (and Watford General Hospital, where we plan to give birth), they measure one of the four pockets of the amniotic fluid volume, but some hospitals will measure all pockets. As I was measuring on top of the normal range, I was advised to control the sugar in my diet, as above 8cm could be an indicator of gestational diabetes. I have been so good with sugar until the last trimester, but now I have to get myself off it again. But to hear I was 7.7cm was a good trigger to watch my diet for the next ten weeks.
Waist and tummy
Dalson moved on to measuring our girl’s waist (Abdominal Circumference), and I was asked to turn to the other side as the baby was dancing away. We saw a bird’s-eye view of the tummy.
Spine and kidneys
They check the kidneys to assess for normality and also exclude renal pelvis dilation (RPD)—excess fluid inside the foetal kidneys. The fluid measured within the normal range.
Stomach and bladder
Dalson checked the stomach and bladder to ensure the baby was drinking well and the stomach was below the diaphragm. Pregnant women can still catch late-onset Congenital Diaphragmatic Hernia, where the baby’s stomach migrates into the chest. Thankfully, the stomach was where it should be, below the diaphragm.
Heart
We saw the beating heart, which was so relieving to see.
Gender check
It was confirmed again that we were having a girl, and this time I saw the three lines!
Placenta
My placenta was on the back wall, which is good. Dalson checked the blood flow in the umbilical cord to assess fetoplacental circulation, as I had mentioned to her my baby’s reduced movements. There was a normal flow pattern, and the pulsatility index (PI) reading was within the normal range, which was relieving. Indicators for performing umbilical artery Doppler may depend on individual hospital protocols. Some hospitals will check blood flow throughout the Growth scans,, and others will only check if indicated.
Weight
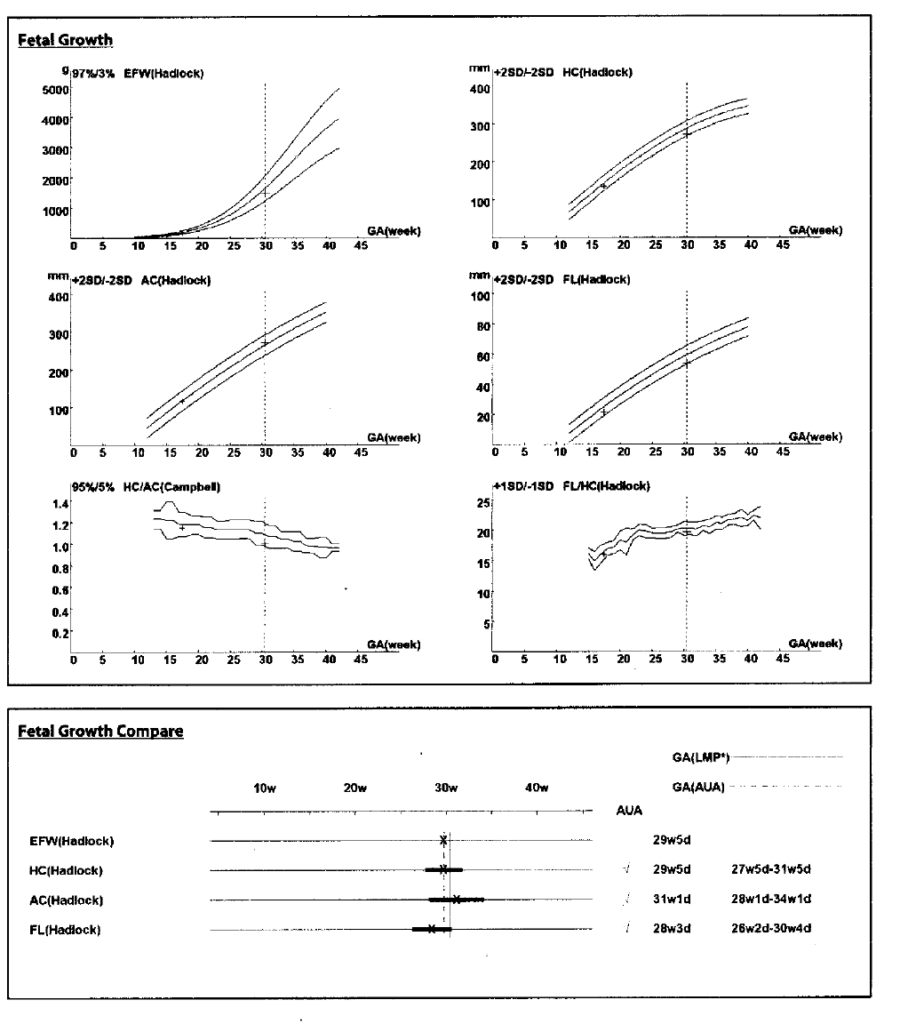
Once Dalson performed all three measurements, the baby weighed 1.5kg/3lbs and 5oz at 31 weeks.
We were provided with a report showing the baby’s measurements and developments, as well as the health and state of my placenta and amniotic fluid. The femur length was showing a little under, but thankfully, the estimated foetal weight (EFW) was plotting within the normal range.

Your questions
When do you have growth scans in pregnancy?
A growth scan is a third-trimester scan to measure whether the baby is growing normally.
How accurate are growth scans?
“They’re not [technically] measuring growth. We don’t measure growth and there is no system by which we can accurately assess the growth – growth is speed, yeah? These are assessment scans or wellbeing scans as we call them.”
Professor Basky Thilganathan, a Consultant Obstetrician and spokesperson for the Royal College of Obstetricians and Gynaecologists (RCOG)
Many readers’ questions revolved around the accuracy of growth scans in the third trimester and whether they were routine or required.
Here were more of your questions:
- How accurate are growth scans?
- Are growth scans common?
- Are growth scans routine?
- Are growth scans safe?
- Are growth scans necessary?
- Are growth scans normal in pregnancy?
- Are growth scans reliable?
- Why would you have growth scans?
- When should growth scans start?
- Does everyone get growth scans?
- Why are growth scans needed?
- Can growth scans be wrong?
- Can growth scans prevent stillbirth?
- Can I refuse growth scans?
I’ll answer all these together. As mentioned above, growth scans are not routine,, but your consultant, doctor or midwife may book a baby Growth scan if you are measuring big or small for dates. The scanning of a baby can show up indicators of too much or too little amniotic fluid and check for other developmental issues, therefore it is important to attend your growth scan if it has been suggested for you to do so. Depending on your issues, you can have a 28 week Growth scan (often when the bump is small) or a 32 week Growth scan (or at 34 and 36 weeks when baby could be measuring too big or too small). I had my initial NHS Growth scan at 36 weeks, so it depends on when your hospital books the appointment.
Growth scans are safe, but as with anything, they are not 100% accurate, as they are based on estimates. Specific issues can be missed at your scan,, so it’s essential to track your baby’s movements and attend all midwife and consultant appointments for optimum antenatal care.
Reasons why you will be offered a growth scan
- If your fundal height (vertical measurement of your belly) is smaller or larger than expected for your baby’s gestational age
- If you have any maternal diseases like diabetes or gestational diabetes
- If your placenta is looking low at the 20-week scan
- If you have a history of pre-eclampsia (high blood pressure and swollen hands, face and feet)
- If you have a history of premature births
- If you are very overweight and you have a BMI of 40 or over
- If there is a large difference in your and your partner’s height, although experts dispute this so it may be assessed on a case-by-case basis
- You have concerns about your baby’s pattern of movement or reduced movements
- You have any vaginal bleeding
- You experience any abdominal pain
Are growth scans 3D or 4D?

At MyBaby4D, you can request a 3D or 4D preview, but the NHS does not offer them. Remember, the growth scan is to check the baby’s well-being and development—all other perks are added bonuses but may not be offered if they disrupt the baby’s well-being check during the appointment.
Can partners attend growth scans?
At MyBaby4D, you are allowed to bring one partner with you, but they advise you to keep children away. The NHS scans I have attended so far do not allow a partner to attend the scan appointment, but this may soon change as restrictions lift in the coming months. Check with your local hospital and stay updated on current COVID rules at MyBaby4D’s website here.
Growth scan cost at MyBaby4D
To book your growth scan at MyBaby4D, please visit here for more details. At the time of this published article,, the price is currently £65.00, but may be subject to change.
* I was offered a Growth & Presentation Scan for the review article but all words and opinions are 100% my own
*MyBaby4D Watford is a trading name of Ultrasound Image Studio Ltd