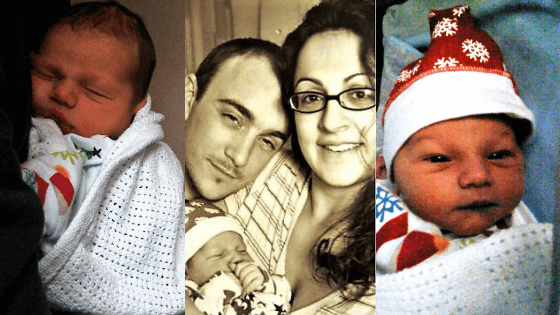
Aron’s crash C section traumatic birth story
This is Aron’s crash C section traumatic birth story, so there are some trigger warnings if you are sensitive to birth. It was a happy outcome and my baby is now twelve, but the details of the birth were traumatic. If you’ve had birth trauma, it’s important to seek help and talk through your birth with a medical professional. Contact the Birth Trauma Association for advice.
I started having contractions on Friday at 3.30am, and these were fairly mild – a bit like the stomach pain you get from diarrhoea. So, it didn’t occur to me that these could have been the start of contractions, even though my due date had already passed a week ago.
I tried not to wake hubby the first time I went to the loo, but by the second time, half an hour later, hubby shot up in bed and asked me if the contractions had started. I replied honestly that I didn’t know, but the pain was coming every half an hour, so we both deduced that these were contractions and hubby stayed home instead of going to work that day
By Saturday at 4 am the contractions were coming every 15 minutes and the pain was situated only in my back. They felt less like diarrhoea pains now and more like a backache you get when you’re on your period. When I went to the birth centre to be assessed, as I felt like I was in labour for a while, the midwife said that my cervix was closed and I was still in the very early stages of labour.
These contractions were becoming steadily worse, but they were still manageable if I concentrated on the breathing techniques I had learned during my pregnancy. So we went home, but by Saturday at 11 pm, I was in absolute agony and my back pain was excruciating to where I couldn’t just breathe through the pain anymore.
I contacted the birth centre again, only to find out they would be closed for the weekend because of the snow, but the lady on the phone heard me having a contraction and advised me to come into the local hospital ASAP. The medical staff monitored my contractions and the baby’s heart on a monitor by a hospital bed, which I couldn’t stop staring at, and they examined me internally to find out that I was only 2 cm dilated.
They told me they were concerned about the baby’s heartbeat, which kept dipping after every contraction. This worried the doctors a little, but they assured me that things should be fine, so they gave me gas and air and codydramol for the back pain and I was told to come back at 9am that morning to monitor the baby’s heartbeat again.
By 9am I was almost screaming from the back pain and when we got to the hospital we were told to wait in the waiting room for over an hour until a room opened up. Hubby was visibly worried at the sight of me during my contractions and extremely annoyed at the staff because one room was taken up by a couple who were planning to have an induction, so hubby complained to a member of staff that my situation was far worse than theirs and that we should have that room.
Aron’s crash C section traumatic birth story begins
That member of staff agreed and told the couple to vacate the room so that I could lie in bed. But after an hour and a half of waiting, I was inconsolable at that point, begging for some pain relief. The midwife couldn’t even give me gas and air because there weren’t any spare cylinders, so I was just screaming inside at the pain now. It felt like the baby was hitting a nerve on my back and the pain lingered on after every contraction. The midwife brought another heart monitor into the room and I glimpsed her worried face and asked her what was wrong.
She replied she had to, “Call a doctor in as the baby’s heartbeat had dropped significantly.” Almost instantaneously I was rushed into an emergency room where there were a group of doctors and midwives running around me trying to sort something out, but no one was telling me anything. I started crying because I was so scared, plus the pain was unbearable. Luckily, the baby’s heartbeat started returning to normal, and they found me some gas and air.
By 5 pm on Sunday, I was progressing slowly and the gas and air were not doing anything to relieve the pain anymore. The Doctor came in and told me he thought I should have an emergency caesarean section because the baby was getting distressed after every contraction. They gave me crash c-section anaesthesia and epidural and I was rushed into the theatre room.
I had no idea what the crash caesarean section protocol was but the emergency cs was the worst thing I had ever, ever dealt with. I felt everything without the pain. It felt like someone was pushing my organs around and I was crying so much, I just wanted to leave the theatre room. I heard the surgeon say that the cord was wrapped around the baby’s neck twice.
At 5.19pm little Aron was born but he had to be checked over as the cord that had been wrapped around his neck had pulled his head back, so every time he tried to come out naturally, his head would hit my spine instead, causing that insanely painful backache. Also, every time the cord was pulled after every contraction, my placenta had come away and rupture. So the longer he was in my tummy, the longer we were endangering both of our lives.
The midwife told me that if they had waited any longer, then an entirely different outcome would have arisen hence the crash caesarean. I’m not sure if she was trying to make me feel better by saying that, but I guess I can count my lucky stars! He would never come out naturally because of the cord and the placental abruption.
I’m glad we had called the birth centre and had been advised to go to the local hospital that night, as I dread to think what might have happened if we didn’t. Whatever the reasons for emergency c section, after 3 days of intense pain and 2 days of recovery at
As far as difficult birth stories, in hindsight, this one was the worst. But, I’m recovering slowly after the emergency c-section trauma and have a lot of stitches. My haemoglobin levels have gone down to 9.2 because I lost so much blood during the birth, but I’m a tough cookie and fighting fit now.
After everything that had happened with the emergency caesarean delivery, I would still do it again because something so beautiful came out of it.
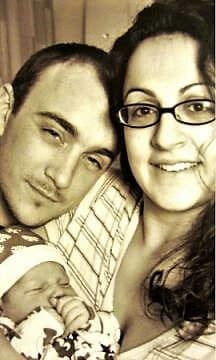
I have never been more proud of my baby. Plus, if it wasn’t for the staff at the hospital acting so quickly to save my baby, my hubby, my best friend and my family around me, I think I would have definitely fallen apart and little Aron may not have been here.
So I welcome little Aron into the world, born on 19 December 2010 at 17.19 and weighing a healthy 8lbs 9oz/3.79kg. I can already see that he has my skin and hair colour and he seems very relaxed.
I now can’t wait to jump into the next chapter of my life – the personal and life-changing story of motherhood.
Read my journey to motherhood here – 1 week old!
For more labour and birth stories (including birth trauma stories, giving birth naturally stories, and c section stories), click here!
Have you had a stressful childbirth experience or know anyone with bad birth stories? Please share your story here.
FAQ
Crash c-section vs emergency c-section. What’s the difference?
Other questions asked were:
- What is a crash c-section?
- What causes a crash c-section?
- How long does emergency c section take?
- How long does an emergency c section take?
- How fast is a crash c-section?
- What does emergency c section mean?
- What does a crash c section mean?
- How long does a crash c section take?
- When is emergency c section needed?
- What is a crash emergency c section?
- What causes emergency c section?
- What is a crash caesarean section?
- What is an emergency Csection?
- Why might you need an emergency Csection?
- Common causes for an urgent Csection?
- Common causes for emergency Csections?
- What happens if I need to have an emergency Csection?
- Indications for emergency caesarean section?
- When might an emergency caesarean section be needed?
- What’s the difference between the types of Csections?
- How common is caesarean section?
- Reasons for an unscheduled Csection?
- Reasons for an emergency Csection?
- What is a crash c section?
- What are emergency caesarean sections?
- What are the causes for c section?
Both crash c-sections and emergency c-sections are medical interventions performed during childbirth when there are complications or concerns about the safety of mum or baby. While the terms “crash c-section” and “emergency c-section” are sometimes used interchangeably, they can have slightly different meaning.
“Crash c-section” is often used in emergency medical settings or in situations where there is an immediate threat to the life of mum or baby. It implies that the situation is critical and requires immediate surgical intervention. This can occur when there is severe foetal distress, sudden maternal complications (such as placental abruption or uterine rupture), or other life-threatening emergencies.
An emergency c-section refers to a situation where there is a need for an unplanned caesarean delivery because of a sudden change in mum or baby’s condition. This can include scenarios where there are concerns about the baby’s heart rate, problems with the progression of labour (such as failure to progress or stalled labour), maternal health issues (such as preeclampsia or severe bleeding), or other unexpected complications that require immediate intervention.
In both cases, the decision to perform a crash or emergency c-section is made by the medical team based on their assessment of the situation and how urgent the intervention needs to be.
How common are crash c-sections?
Statistics for crash c-sections are difficult to find but emergency c-sections, which encompass both planned and unplanned emergency situations, are a common occurrence in obstetric practice. The Royal College of Obstetricians and Gynaecologists (RCOG) in the UK reports that emergency c-section rates can range from around 15-25% of all deliveries.
Not all emergency c-sections are “crash” c-sections. The decision to perform a c-section, whether planned or unplanned, is based on the healthcare provider’s team and their assessment of the health and safety of mum and baby.
For more information on crash c-section rates in the UK, consult official reports, research studies, or reach out to healthcare professionals or organisations specialising in maternal health and childbirth statistics in the UK, such as the National Health Service (NHS) or the RCOG.
What is a traumatic birth story?
A traumatic birth story is a physically and/or psychologically distressing experience during childbirth that can leave a lasting emotional impact. Hard birth stories generally leave the person feeling like they’ve lost power and control and are in a place of fear during emergency labour and delivery.
What are examples of a traumatic birth?
Other questions asked were:
- What are some traumatic birth stories?
- Are there any difficult birth experience stories?
- What are examples of birth horror stories?
- What are examples of birth injury stories?
- Do you have any birthing stories which have been traumatic?
- Where can I find childbirth stories which were difficult?
- Do you have any difficult labour experience stories?
- Do you have any painful childbirth stories?
- Do you have any pregnancy delivery stories?
Some birth trauma examples may include:
- An emergency situation like foetal distress, placental abruption, emergency c-section scar ripping, or cord prolapse
- Prolonged or stalled labour
- Medical interventions which can be excessive, like inductions, the emergency c-section procedure, forceps or vacuum extraction, or episiotomies
- Perceived lack of support, feeling unheard by healthcare professionals, or having preferences disregarded during labour and birth
- Maternal health complications like pre-existing health conditions or pregnancy complications, like preeclampsia or gestational diabetes.
- Neonatal complications where the baby experiences health issues or requires intensive medical care after birth
What is the most common birth trauma?
One of the most common types of birth trauma is perineal trauma or perineal tears. The perineum is the area between the vagina and the anus, and during childbirth, it can sometimes tear or be cut (episiotomy) to help deliver the baby. Perineal tears are classified into different degrees based on their severity:
- First-degree tear: This is the mildest form of perineal tear, involving only the skin around the vaginal opening.
- Second-degree tear: This tear extends beyond the skin and involves the vaginal tissue as well.
- Third-degree tear: This tear extends even further into the anal sphincter muscles.
- Fourth-degree tear: This is the most severe type of tear, extending through the anal sphincter muscles and into the rectum.
Perineal tears are relatively common during vaginal delivery, particularly among first-time mothers or where medical interventions, such as forceps or vacuum extraction, are used. Factors that can increase the likelihood of perineal tears include the baby’s size, position, rapid delivery, and the use of interventions like episiotomy.
Not all perineal tears are traumatic for everyone. The experience can vary based on pain, complications, emotional distress, and the overall birthing experience.
Can you get PTSD from a traumatic birth?
Other questions asked were:
- Can a traumatic birth cause PTSD?
- What are the causes of birth trauma PTSD?
- Can an emergency c section cause ptsd?
Yes it is possible to develop PTSD from a traumatic birth. PTSD is a mental health condition that can develop when someone has experienced or witnessed a traumatic event.
The symptoms of PTSD typically fall into four categories:
- Intrusive thoughts or memories: People with PTSD may experience recurrent, distressing memories of the traumatic birth, nightmares, or intrusive thoughts. These could involve reliving the intense pain, fear, or sense of helplessness during the delivery process.
- Avoidance and numbing: You may try to avoid reminders of the traumatic birth experience, such as avoiding discussions about childbirth, medical settings, or even future pregnancies. You may also feel emotionally numb, disconnected, or experience a reduced interest in activities you once enjoyed.
- Hyperarousal and increased anxiety: This includes symptoms such as irritability, difficulty concentrating, hypervigilance, exaggerated startle response, and difficulties with sleep. These symptoms can continue long after the traumatic birth experience and can significantly impact daily functioning.
- Negative changes in mood and cognition: You may experience negative thoughts about yourself, others, or the world around you. You may struggle with feelings of guilt, shame, or distorted beliefs related to the traumatic event.
Not everyone who experiences a traumatic birth will develop PTSD. However, if you are, then seek professional help from mental health professionals experienced in trauma and perinatal mental health. Therapy such as cognitive-behavioural therapy (CBT), eye movement desensitisation and reprocessing (EMDR), and support groups can help you process the trauma, manage symptoms, and promote recovery.
Was our birth so traumatic for us that we can’t remember it?
It is possible for birth to be so traumatic that your memory of the event may become fragmented, vague, or even completely absent. A traumatic birth and labour story can trigger a defence mechanism known as dissociation, which can affect memory recall. Dissociation is a psychological response that can occur during distressing or overwhelming events as a way to protect yourself from the full impact of the trauma.
Memory recall can vary from person to person. Some women may have a clear recollection of their birth experience, while others may have only limited memories.
If you have concerns about your birth experience and its impact on your memory, speak to a mental health professional or a healthcare provider who can provide medical advice and support tailored to your specific situation.
How do doctors feel when a patient unexpectedly comes close to dying? I recently had a traumatic birth experience. I want to ask my OB how this has impacted him, but I’m afraid. Would doctors be open to this kind of conversation with their patient?
Every doctor’s emotional response is unique, but their primary focus is to provide medical care to ensure the best possible outcome for their patients. Doctors are trained professionals who understand that empathy and compassion for their patients is very important.
It is perfectly acceptable to have a conversation with your OB about your traumatic birth story and ask if they are open to discussing it. Talking about your feelings with your OB can help them understand your situation and promote healing. They may even recommend you seek support from a mental health professional for more specialised guidance and offer additional information on what to do next.
What is it like to remember a traumatic twilight birth?
A twilight birth refers to when a mother receives medication to induce a state of semi-consciousness or mild sedation during labour. While this helps to manage pain and discomfort it can cause hazy memories of birth.
Traumatic births can involve complications, high levels of pain and medical interventions and this can cause:
- Flashbacks which can be triggered by specific sounds and smells associated with birth
- Anxiety and fear, especially when thinking about future pregnancies or medical procedures.
- Sadness when remembering the pain or complications during birth, which could lead to postnatal depression
If someone survives a major transitional traumatic experience at birth when both the baby mother almost died from complications of the childbirth labour unexpectedly, how would this affect effect the mother of the child?
Experiencing a major transitional traumatic experience during childbirth where both the baby and mother face life-threatening complications can have a real impact on mum’s emotional wellbeing. This can cause emotional trauma, anxiety and fear, depression and mood disorders, guilt and self-blame, bonding difficulties and a negative outlook on future pregnancies.
It is important to seek professional help from therapists, healthcare providers, and/or support groups specialising in perinatal mental health. They can provide the appropriate support to help mum navigate her emotions, process the trauma and begin the road to heal.
Does a traumatic birth negatively affect a baby’s development?
Other questions asked were:
- Is birth traumatic for the baby?
A traumatic birth could potentially have a short-term and long-term effect on baby’s development. but it very much depends on the birth itself, the severity of the trauma, child health and the support provided after birth.
Some potential effects could include:
- Oxygen deprivation may cause an injury to organs, brain damage or other complications that require medical intervention and ongoing monitoring
- Some studies suggest that traumatic births may contribute to emotional and behavioural difficulties in children. They may be at a higher risk of experiencing anxiety, hyperactivity, sleep disturbances, and other behavioural challenges, although there are many factors that would contribute to a child’s emotional and behavioural development.
- There is limited research specifically focusing on the impact of a traumatic birth on cognitive development. Some studies suggest that certain types of birth trauma like oxygen deprivation, may have long-term effects on cognitive functioning.
- A traumatic birth experience may affect the bonding and attachment process between baby and parents.
Not all outcomes are negative or permanent and with the right support and care, babies can overcome the initial impact of a traumatic birth and develop normally.
If you are concerned about the effects of your traumatic birth on your baby’s development, consult your paediatrician or child development specialist for an individual assessment of your baby.
Is adoption at birth traumatic for the baby? Why he doesn’t even remember the experience, so why should it affect him?
Adoption at birth can be a complex and emotional experience for both the baby and the birth parents. While it is true that the baby may not have conscious memories of the adoption process itself, it doesn’t mean that the experience is without potential impacts.
The separation from birth parents, especially from mum, can be a significant emotional event for a newborn. Babies have a natural instinct to seek proximity and connection with their primary caregivers and the sudden separation could lead to distress and feelings of loss.
Early experiences also shape the brain and infancy is a very critical period for brain development. The quality of care, consistency and responsiveness of adoptive parents can influence the baby’s attachment patterns and emotional development.
Even without conscious memories, a baby may still experience a sense of loss or disconnect with birth parents. As the child grows older and becomes more aware of their adoption, they may ask questions and this could evoke emotions which may require extra support and understanding from adoptive parents.
Some children may face attachment difficulties and feelings of abandonment.
If adoption at birth is traumatic for the baby, is birth via surrogate traumatic too? Why do people feel that adoption should be open but surrogacy need not be?
The experience of birth via surrogate can be complex and emotionally charged, both for the intended parents and the surrogate mother. Babies have an innate need for attachment and connection and the sudden separation can be emotionally challenging for them.
The immediate post-birth period is crucial for bonding and attachment between baby and primary caregivers. In traditional surrogacy arrangements, where the surrogate is genetically related to the baby, the separation may be difficult, so the intended parents must provide quality and consistent care to support healthy bonding and attachment.
As the child grows older, they may have questions about their biological family and will want to understand their identity. They have may have more complex questions or feelings so it’s important to be open and honest when addressing their concerns.
Regarding the question of open adoption versus open surrogacy, perspectives can vary among individuals and cultures. Some people advocate for open adoption, where there is ongoing contact and information sharing between the birth parents and the adoptive parents, as they believe it can benefit the child’s wellbeing.
Some people may feel that surrogacy is primarily a contractual arrangement focused on fulfilling the intended parents’ desire to have a child, and they may not see the same need for ongoing contact or open relationships. However, there are also instances where intended parents and surrogates choose to have ongoing contact and maintain a relationship, similar to open adoption.
Ultimately, decisions regarding openness in adoption and surrogacy should be made based on the best interests of the child. It’s important for intended parents, surrogates, and all parties involved to have open and honest discussions, consider the emotional wellbeing of the child, and seek guidance from professionals specialising in adoption or surrogacy.
Do infants experience trauma when separated from their biological mother, i.e. Primal Wound?
The concept of the “Primal Wound” is a theory by Nancy Verrier in her book of the same name. It suggests that the separation of an infant from their biological mother, particularly through adoption, can lead to a deep and lasting emotional wound or trauma.
However, this theory is not universally accepted or supported by all psychologists and child development experts.
The experience of separation from the biological mother can be emotionally challenging for a baby, as it disrupts the natural bond that forms during the early stages of life. Babies have a natural need for attachment with their primary caregivers, and the sudden separation can lead to feelings of distress, loss, and confusion.
Not all babies will experience long-lasting trauma and many adopted children grow up in loving and supportive families, where they form secure attachments. With nurturing care, open communication about adoption, and support from professionals specialising in adoption and child development, the potential negative effects of separation can be reduced.
I can’t forget the horror of my son’s birth. How do I forget?
Other questions asked were:
- I want to start learning and growing from my experience with birth trauma. What steps do I take to the road to recovery?
- How do I look after my mental health after emergency Csection?
I’m really sorry to hear you’re struggling with the memories of your son’s birth. While it may not be possible to completely forget a traumatic experience, there are ways to help you cope with and reduce its impact. Here are some suggestions:
- Reach out to a mental health professional, such as a therapist or counsellor, who specialises in trauma or perinatal mental health. They can provide appropriate guidance, support, and therapeutic techniques to help you process the reasons for c section or normal birth and the memories in a healthy way.
- Share your feelings with a trusted friend, family member, or support group. Talking about your trauma can help alleviate the burden, provide perspective, and offer emotional support.
- Engage in activities that promote your wellbeing and help manage traumatic stress. This can include regular exercise, mindfulness or meditation, pursuing hobbies or interests you enjoy, and getting good sleep.
- Surround yourself with supportive people who can empathise with your situation. Joining support groups, either in-person or online, specifically focused on birth trauma or perinatal mental health, can connect you with others who may experience birth trauma too.
- Trauma-focused therapies, such as Eye Movement Desensitisation and Reprocessing (EMDR) or Cognitive Behavioural Therapy (CBT), can help address traumatic memories and distress. A trained therapist can guide you through these evidence-based therapies.
- Writing about your feelings in a journal can be a therapeutic way to process and release your thoughts. It can help gain insight, a sense of control, and promote emotional healing. You can even enjoy healing through storytelling.
I had an emergency c section. Can I have a vaginal birth now?
Other questions asked were:
- Emergency Csection and future pregnancies. Can I give birth naturally?
In the UK, the possibility of a VBAC after a previous emergency c-section is considered viable for many women but it does depend on certain factors, such as:
- Previous c section details, i.e. a low transverse incision is associated with more successful VBAC outcomes compared to vertical or classical incisions.
- Your overall health, including any underlying medical conditions, will determine if it’s safe for you to have a VBAC.
- Your current pregnancy may determine if a VBAC is possible, i.e. the position of the baby and the gestational age.
- Hospital resources may not be so readily available to support VBAC, including access to an operating room in case of an emergency.
Is emergency c section worse than planned?
This is a subjective question as sometimes each c section has their own benefits and considerations, for example:
Emergency c sections are performed when there is a need for medical intervention because of the health and safety of mum and baby. The unexpected nature of the emergency c section can invoke anxiety. The sudden change in birth plans can create a sense of urgency too and offer less time for emotional and mental preparation.
Scheduling a planned c section allows for better planning and preparation. You have a better sense of control and readiness for the procedure too. You may feel more at ease emotionally because you’ve had time to discuss and understand the process with your hospital. You can also discuss parts of the surgery which involve more attachment like cutting the umbilical cord or enjoying skin-to-skin straight after delivery.
In some cases a planned c section may offer a more controlled environment for recovery as there is time to discuss post-operative care and pain management strategies in advance.
Is emergency c section covered by insurance?
In the UK, emergency c-sections are generally covered by the NHS, which provides free healthcare services, including emergency medical interventions.
In the US, coverage for emergency c-sections may vary depending on the specific health insurance plan. Most health insurance plans cover medically necessary procedures, including emergency caesareans. Review the terms and conditions in your insurance policy, including any co-pays, deductibles and coverage limitations to understand whether emergency c-sections are covered. You can contact your insurance provider for up to date information and ask the hospital billing department for help in understanding the potential costs.
Is emergency c section dangerous?
Other questions asked were:
- Is emergency c section safe?
- Is an emergency c section major surgery?
- Is an emergency c section bad?
- Why c-section is bad?
- When did c sections become safe?
- Can a baby die during c section?
- What are the risks of an emergency Csection?
- Risks involved during and after an emergency Csection?
- What causes death during c-section?
- What are the risks of a caesarean section?
- How safe is a c section?
Emergency c-sections, like any surgical procedure, carry risks and potential complications. However, emergency c-sections are necessary if there are any risks to the mum and/or baby. Therefore, in most cases, the benefits of having a c section outweigh the risks.
What day is worse after c section?
Other questions asked were:
- What is recovery like after an emergency Csection?
- What to expect during an urgent Csection?
- What to expect during an emergency Csection?
- What to expect after an emergency Csection?
- What is the recovery after emergency Csection?
- How will I feel after a caesarean section?
- What is a caesarean section like?
Recovery after you have an emergency c-section (or planned) can vary from person to person, and there isn’t a universally agreed-upon “worst” day. However, there are certain common patterns that some mums may experience during their recovery. Here are some general milestones:
- The first few hours following a c-section can be difficult as the effects of anaesthesia wear off and you feel the initial pain and discomfort. You may also feel nausea, groggy and sore around the incision site.
- Day 1-2: Moving around, coughing, sneezing, and laughing may be particularly uncomfortable. Many people require pain medication during this period.
- Day 3-4: The pain and discomfort may begin to improve around this time. However, fatigue and limited mobility are still common, so keep practicing good self-care and following the instructions provided by the hospital.
- Day 5 and beyond: By this point, you will begin to notice an improvement in your overall wellbeing and have reduced pain and increased mobility.
However, an individual recovery of delivery time can vary, so listen to your body and gradually increase your activity level as advised by your hospital.
Will I be awake for a caesarean section?
In most cases, during a c-section, you are conscious under local anaesthetic, typically in the form of an epidural or spinal block, which numbs the lower half of the body. This allows you to be aware of your baby while ensuring you don’t feel any pain.
You may experience sensations such as pressure, tugging or movement during the surgery. If this is uncomfortable you should let the healthcare team i.e. the anaesthetists, obstetricians and nurses know. They will explain the process and provide reassurance throughout the procedure.
There may be rare emergency situations where general anaesthetic is needed, which means you’ll be unconscious. This may be if a local anaesthetic isn’t feasible or poses additional risks.
Make sure you understand the different anaesthesia options and discuss with your hospital what you prefer so you feel well-informed before your planned c-section.
How long does a caesarean section take?
Other questions asked were:
- What will happen during an emergency Csection?
In general, a c-section takes around 45 minutes to an hour from the time the surgical incision is made to the completion of the procedure, depending on whether there are any emergency issues.
Before they start the surgery, the healthcare team will prepare the operating room and mum for the procedure, including positioning, administering anaesthesia and making sure all necessary equipment is in place. This takes around 15-30 minutes
Then once the prep is complete the surgeon will make the incision in the abdomen and the uterus to access the baby. The baby is then carefully delivered through this incision. This take around 10 – 20 minutes.
After the baby is delivered, the team will remove the placenta, inspect the uterus and close the incision. This part takes around 10-20 minutes.
Can emergency c section cause infertility?
A C-section is not known to cause infertility, although, as it is surgery, it may carry some risks, such as infection or complications related to anaesthesia. However, infertility is not typically one of the long-term effects associated with c-sections.
However, certain medical conditions, complications during childbirth, or pre-existing fertility issues could be related to difficulties conceiving in the future, but these are not directly caused by the c-section procedure itself.
Can an emergency c section cause autism?
There is no scientific evidence to suggest that an emergency c-section directly causes autism. Autism is a complex neurodevelopmental condition that is believed to have a multifactorial aetiology, involving a combination of genetic, environmental, and possibly prenatal factors. The exact causes of autism are still not fully understood.
While certain prenatal and perinatal factors have been studied for their potential association with autism, the link between c-sections and autism is not well-established. Research in this area has yielded inconsistent results, with some studies suggesting a small association between c-section delivery and an increased risk of autism, while others have found no significant association.
If you have questions or concerns about the potential risk factors for autism or any other developmental conditions, seek guidance from healthcare professionals who can provide personalised advice based on your specific situation and medical history.
How many caesarean sections can I have?
In the UK and the US, the number of c-sections a person can have may vary depending on several factors, including medical history, the specific circumstances of each pregnancy, and healthcare providers’ recommendations. Currently there is no set limit on the number of c-sections a person can have.
In the UK, the National Institute for Health and Care Excellence (NICE) guidelines state that a woman’s preference for a VBAC should be respected and supported, and the decision should be made through shared decision-making between mum and healthcare provider. NICE guidelines also suggest that a planned c-section should be offered to women who have had more than two previous c-sections.
In the US, the American College of Obstetricians and Gynaecologists (ACOG) acknowledges that VBAC can be a safe option for many women with one or even two previous c-sections. However, the decision about the mode of delivery after a previous c-section should be individualised, taking into account factors such as the type of uterine incision, previous complications, and current pregnancy considerations.
It’s important to note that the specific recommendations and practices may vary among healthcare providers and hospitals and a careful assessment of the individual’s medical history and current circumstances is made first before coming to a decision.
What is the pain relief after caesarean section?
Other questions asked were:
- Do emergency c-section births hurt?
Pain relief options after a c-section in both the UK and the US generally involve a combination of medications to manage pain and promote recovery.
In the UK, after a c-section, pain relief is typically provided through a combination of analgesic medications. This may include intravenous (IV) pain medications such as opioids (e.g. morphine) given during and immediately after the surgery. In addition, oral or intravenous nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to help control pain and reduce inflammation in the days following the procedure. Local anaesthesia techniques such as epidurals or spinal anaesthesia are often administered during the c-section surgery to numb the lower body and provide pain relief.
In the US, pain relief options after a c-section are similar. Opioid medications may be used to manage pain, either through IV administration during and immediately after the surgery or through oral medications in the days following the procedure. NSAIDs may also be prescribed to help with pain control and reduce inflammation. Regional anaesthesia techniques, such as spinal anaesthesia or epidurals, are aso used during c-sections to provide pain relief during and after the surgery.
The choice of pain relief methods and medication may vary based on individual circumstances, the preference of the healthcare provider, and the hospital’s protocols.
Is caesarean section safer for very premature babies?
For very premature babies, the decision regarding whether to have a caesarean section (c-section) or vaginal birth, is based on the circumstances of each individual case.
In some cases, a c-section may be considered safer for very premature babies due to the potential risks associated with vaginal delivery. For example, if there are concerns about the baby’s position, the ability to tolerate the stress of labour, or the potential for birth complications, a c-section might be recommended to ensure a safer delivery.
Additionally, if there are certain medical conditions or complications that make a vaginal birth risky for the mother or the baby, a c-section might be the preferred option. These conditions can include placenta praevia (when the placenta partially or fully covers the cervix), certain types of uterine abnormalities, or concerns about the baby’s health.









4 Comments